Paroxysmal atrial fibrillation is a subtype of atrial fibrillation characterized by sudden and recurrent episodes of irregular heart rhythm that typically resolve on their own within 7 days, often within 24 hours. These episodes can occur sporadically and without warning, potentially progressing into more persistent or permanent forms of AFib if not effectively managed. It is a major clinical concern due to its association with stroke, heart failure, and reduced quality of life.
Pathophysiology of Paroxysmal Atrial Fibrillation
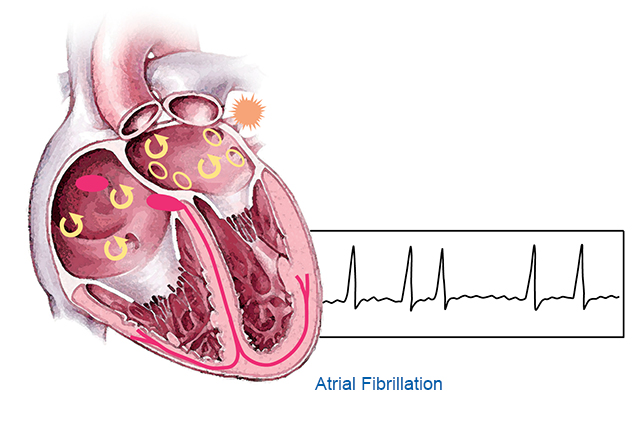
In paroxysmal AFib, electrical signals in the atria become chaotic, causing the upper chambers of the heart to quiver instead of contracting effectively. This irregularity often originates in ectopic foci, primarily located in the pulmonary veins.
Key Mechanisms:
- Electrical remodeling of atrial tissue
- Abnormal automaticity from pulmonary veins
- Structural changes due to fibrosis or inflammation
- Autonomic nervous system imbalance
Causes and Risk Factors for Paroxysmal AFib
Common Causes:
- Hypertension
- Coronary artery disease
- Valvular heart disease
- Hyperthyroidism
- Sleep apnea
- Acute infections
- Alcohol use (“holiday heart syndrome”)
Major Risk Factors:
| Category | Risk Elements |
|---|---|
| Cardiovascular | Heart failure, myocardial infarction |
| Lifestyle | Smoking, excessive alcohol, high stress |
| Systemic Illnesses | Diabetes, obesity, chronic kidney disease |
| Age-related | Increased prevalence in individuals >60 yrs |
| Genetic | Family history of AFib |
Symptoms of Paroxysmal Atrial Fibrillation
While some individuals remain asymptomatic, many experience noticeable episodes of cardiac distress. Symptoms can vary in frequency, severity, and duration.
Common Symptoms:
- Palpitations or fluttering in the chest
- Sudden onset of fatigue
- Shortness of breath
- Chest discomfort
- Lightheadedness or dizziness
- Anxiety
- Weakness, especially with exertion
Diagnosis of Paroxysmal AFib: Clinical and Technological Tools
Timely and accurate diagnosis is critical to prevent complications like stroke or heart failure. Paroxysmal AFib may evade detection due to its intermittent nature.
Diagnostic Methods:
- Electrocardiogram (ECG): Detects abnormal atrial activity during episodes
- Holter Monitor: Continuous monitoring over 24–72 hours
- Event Monitor or Implantable Loop Recorder: For longer-term detection
- Echocardiography: Evaluates cardiac structure and function
- Blood Tests: Assess thyroid function, electrolyte levels, and markers of inflammation
Classification of AFib by Duration and Pattern
| Type of AFib | Description |
|---|---|
| Paroxysmal | Episodes terminate spontaneously, <7 days |
| Persistent | Requires intervention to restore sinus rhythm |
| Long-standing Persistent | Persists for >12 months without interruption |
| Permanent | Sinus rhythm restoration not attempted or failed |
Management and Treatment of Paroxysmal Atrial Fibrillation
Effective management involves addressing symptoms, reducing recurrence, and preventing thromboembolic events. Treatment options vary based on individual risk profiles and comorbidities.