Parkinsonism refers to a group of neurological disorders characterized by symptoms similar to those of Parkinson’s disease. These include bradykinesia, rigidity, resting tremor, and postural instability. While Parkinson’s disease is the most well-known cause, other neurodegenerative and secondary conditions may also lead to parkinsonian features.
Parkinsonism is not a diagnosis but a clinical syndrome, and identifying the underlying cause is essential for appropriate treatment and management.
Key Features and Symptoms of Parkinsonism
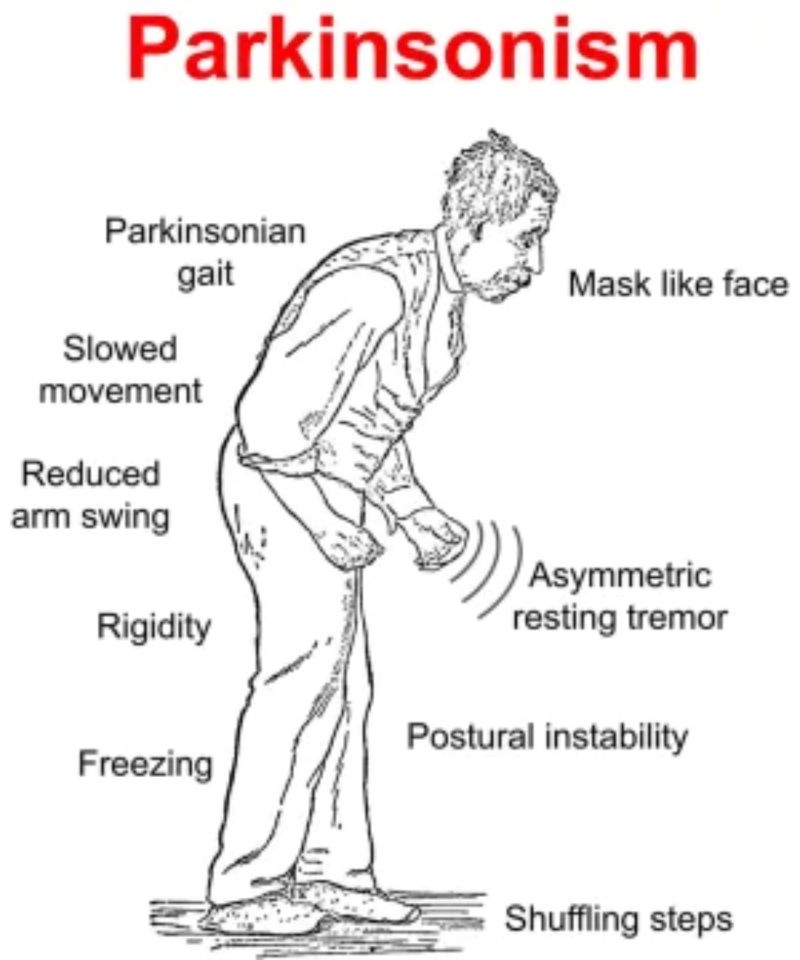
The clinical presentation typically involves motor symptoms, although non-motor symptoms often coexist.
Core Motor Symptoms
- Bradykinesia: Slowness of movement, a hallmark symptom required for diagnosis
- Rigidity: Muscle stiffness, typically affecting limbs and neck
- Resting Tremor: Typically “pill-rolling” in nature, present at rest
- Postural Instability: Impaired balance and frequent falls in later stages
Non-Motor Symptoms
- Cognitive impairment
- Sleep disturbances
- Depression and anxiety
- Autonomic dysfunction (e.g., constipation, orthostatic hypotension)
Types of Parkinsonism: Primary and Secondary
Understanding the classification is critical for prognosis and management.
Primary Parkinsonism
- Parkinson’s Disease (PD): The most common form, characterized by progressive loss of dopaminergic neurons in the substantia nigra.
Atypical Parkinsonism (Parkinson-Plus Syndromes)
- Progressive Supranuclear Palsy (PSP): Features vertical gaze palsy and early falls.
- Multiple System Atrophy (MSA): Involves autonomic failure, cerebellar signs, and parkinsonism.
- Corticobasal Degeneration (CBD): Marked by asymmetric rigidity and apraxia.
- Dementia with Lewy Bodies (DLB): Parkinsonism with early cognitive decline and visual hallucinations.
Secondary Parkinsonism
- Drug-Induced Parkinsonism: Caused by antipsychotics, antiemetics, or calcium channel blockers.
- Vascular Parkinsonism: From multiple small strokes affecting basal ganglia.
- Toxin-Induced: Exposure to manganese, carbon monoxide, or MPTP.
- Post-Infectious Parkinsonism: Rare, following encephalitis lethargica or viral infections.
- Normal Pressure Hydrocephalus (NPH): Triad of gait disturbance, dementia, and urinary incontinence.
Causes and Risk Factors for Parkinsonism
The etiology varies depending on the type.
Primary Causes
- Idiopathic in Parkinson’s disease
- Genetic mutations (e.g., SNCA, LRRK2)
Secondary Causes
- Medication side effects
- Cerebrovascular disease
- Traumatic brain injury
- Chronic exposure to industrial toxins
- Infections (e.g., HIV, Japanese encephalitis)
Risk Factors
- Age (incidence increases with age)
- Male gender
- Family history (in PD)
- Environmental exposures (e.g., pesticides)
Diagnosis of Parkinsonism: Clinical and Imaging Techniques
An accurate diagnosis is based on clinical features and exclusion of secondary causes.
Clinical Evaluation
- Detailed neurological examination
- Response to dopaminergic therapy (Levodopa trial)
- Assessment of symptom symmetry, progression, and associated features
Imaging Modalities
| Imaging | Purpose | Usefulness |
|---|---|---|
| MRI Brain | Rules out structural causes | Helpful in secondary parkinsonism |
| DaTSCAN (SPECT) | Assesses dopamine transporter levels | Differentiates PD from drug-induced |
| PET Scan | Research-based tool for functional imaging | High sensitivity, limited availability |
Treatment Options for Parkinsonism
Management strategies depend on the underlying cause and symptom severity.
Pharmacological Treatment
- Levodopa-Carbidopa: Most effective for Parkinson’s disease
- Dopamine Agonists: Pramipexole, Ropinirole
- MAO-B Inhibitors: Selegiline, Rasagiline
- COMT Inhibitors: Entacapone
- Amantadine: Reduces dyskinesia
Limitations in Atypical Parkinsonism
Patients with atypical forms often exhibit limited or no response to levodopa, and progression is typically faster.
Management of Secondary Parkinsonism
- Discontinuation of causative drugs
- Control of vascular risk factors
- Shunt surgery for NPH (if applicable)
Non-Pharmacological Interventions
- Physical Therapy: Improves gait, balance, and reduces falls
- Occupational Therapy: Enhances daily functioning
- Speech Therapy: Addresses dysarthria and swallowing difficulties
- Psychological Support: For depression, anxiety, and caregiver stress
Prognosis and Disease Progression
The prognosis varies widely:
- Parkinson’s Disease: Gradual progression, life expectancy may be near normal with proper care
- Atypical Parkinsonism: More rapid decline, earlier onset of disability
- Secondary Parkinsonism: May stabilize or improve if underlying cause is addressed
Parkinsonism vs Parkinson’s Disease: Key Differences
| Feature | Parkinson’s Disease | Parkinsonism |
|---|---|---|
| Etiology | Idiopathic or genetic | Diverse causes |
| Response to Levodopa | Good | Often poor |
| Symmetry of Symptoms | Asymmetric | Often symmetric |
| Progression | Slow | Variable |
| Cognitive Decline | Late onset | Early in atypical forms |
Prevention and Risk Mitigation
While Parkinson’s disease is largely idiopathic, some preventive strategies may reduce secondary parkinsonism risk:
- Avoid unnecessary exposure to neuroleptic medications
- Control vascular risk factors (hypertension, diabetes)
- Minimize exposure to environmental toxins
- Use protective gear to avoid head trauma
Ongoing research focuses on neuroprotective strategies and early intervention in genetically susceptible individuals.
Frequently Asked Questions
What is the difference between Parkinsonism and Parkinson’s disease?
Parkinsonism is a broader syndrome that includes Parkinson’s disease and other conditions with similar symptoms but different causes.
Can Parkinsonism be reversed?
Some forms, such as drug-induced or NPH-related parkinsonism, may improve or resolve if the underlying cause is treated.
How is Parkinsonism diagnosed?
Diagnosis relies on clinical evaluation and imaging techniques to exclude secondary causes and assess dopaminergic function.
What is the best treatment for Parkinsonism?
Levodopa is most effective in Parkinson’s disease. Atypical forms often require supportive and symptomatic treatment.
Is there a cure for Parkinsonism?
Currently, no cure exists. Treatment focuses on symptom control and improving quality of life.
Parkinsonism encompasses a complex array of conditions unified by similar motor symptoms but distinguished by underlying pathology, prognosis, and treatment response. Accurate diagnosis and individualized care are essential for effective management. As research advances, early detection and targeted therapies promise improved outcomes for those affected by this diverse and challenging neurological syndrome.