Parathyroid carcinoma is a rare but aggressive endocrine malignancy originating from the parathyroid glands. It accounts for less than 1% of primary hyperparathyroidism cases yet is a critical differential diagnosis in patients presenting with severe hypercalcemia. The excessive secretion of parathyroid hormone (PTH) leads to markedly elevated serum calcium levels, posing life-threatening systemic complications.
Unlike benign parathyroid adenomas or hyperplasia, carcinoma typically presents with more pronounced biochemical abnormalities and often with a palpable neck mass, bone resorption, nephrolithiasis, and gastrointestinal disturbances. Early recognition and surgical intervention are essential for disease control and improved survival outcomes.
Pathophysiology: Relationship Between Parathyroid Carcinoma and Hypercalcemia
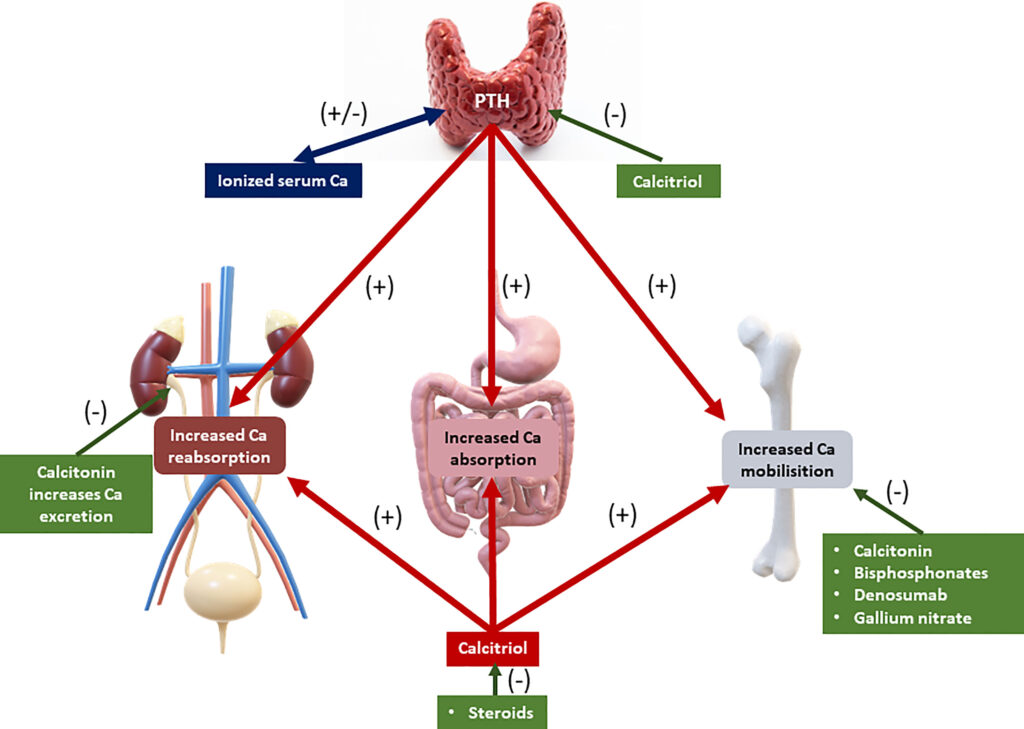
Hypercalcemia in parathyroid carcinoma is driven by autonomous and excessive PTH secretion. This results in:
- Increased osteoclastic bone resorption
- Enhanced renal tubular calcium reabsorption
- Elevated gastrointestinal calcium absorption via calcitriol stimulation
These mechanisms result in sustained hypercalcemia, which can precipitate nephrocalcinosis, renal failure, neurocognitive symptoms, and cardiac arrhythmias.
Clinical Presentation: Signs and Symptoms
Patients with parathyroid carcinoma and hypercalcemia may exhibit the following symptoms:
General and Neuromuscular
- Profound fatigue and muscle weakness
- Depression, confusion, and cognitive decline
- Headaches and lethargy
Gastrointestinal
- Nausea, vomiting, and abdominal pain
- Constipation
- Peptic ulcers and pancreatitis
Renal
- Polyuria and polydipsia
- Recurrent kidney stones
- Progressive renal insufficiency
Skeletal
- Osteitis fibrosa cystica
- Pathological fractures
- Bone pain and deformities
Local Symptoms
- Palpable, firm, non-mobile neck mass
- Hoarseness due to recurrent laryngeal nerve involvement
- Dysphagia or dyspnea in advanced cases
Diagnostic Approach: Identifying Malignancy and Hypercalcemia
Biochemical Evaluation
- Serum Calcium: Often >14 mg/dL in carcinoma
- PTH Levels: Exceeding 3–10 times the upper normal range
- Phosphorus: Typically low due to PTH-induced renal excretion
- Alkaline Phosphatase: May be elevated with bone involvement
- Vitamin D: May be normal or low
Imaging Studies
- Neck Ultrasound: May reveal a hypoechoic, irregular mass with local invasion
- Sestamibi Scan: Assists in localizing hyperfunctioning tissue
- CT/MRI: Useful for evaluating invasion into adjacent structures and metastatic spread
- PET-CT: Indicated in recurrent or metastatic disease for staging
Histopathology and Cytology
Parathyroid carcinoma is definitively diagnosed postoperatively via histological criteria, which may include:
- Capsular and vascular invasion
- Mitotic figures
- Dense fibrous bands
- Trabecular architecture
Fine needle aspiration (FNA) is discouraged due to the risk of tumor seeding.
Differential Diagnosis: Distinguishing from Benign Conditions
Parathyroid carcinoma must be differentiated from:
- Parathyroid adenoma: Smaller size, absence of invasion, less severe hypercalcemia
- Parathyroid hyperplasia: Multiglandular involvement, milder biochemical profile
- Secondary or tertiary hyperparathyroidism: Typically seen in chronic kidney disease
Features strongly suggestive of malignancy include:
- Serum calcium >14 mg/dL
- PTH levels 3–10× upper limit
- Firm neck mass
- Vocal cord paralysis
- Recurrence after initial surgery
Treatment Modalities: Surgical and Medical Management
Surgical Management
En bloc resection remains the gold standard and includes:
- Removal of the affected parathyroid gland
- Ipsilateral thyroid lobectomy
- Surrounding soft tissue excision if invasion is suspected
Avoiding tumor capsule rupture is critical to prevent seeding.
Medical Management of Hypercalcemia
For acute hypercalcemia:
- Aggressive IV hydration with isotonic saline
- Loop diuretics (e.g., furosemide) to promote calciuresis
- Bisphosphonates (e.g., zoledronic acid) to inhibit bone resorption
- Calcitonin for rapid but short-lived calcium lowering
- Cinacalcet, a calcimimetic agent, for PTH suppression
In refractory cases or metastatic disease:
- Denosumab, especially in bisphosphonate-resistant patients
- Radiotherapy or systemic chemotherapy, although efficacy is limited
- Targeted therapy under clinical investigation
Follow-Up and Recurrence Monitoring
Parathyroid carcinoma is notorious for local recurrence and distant metastasis (lungs, liver, bones). Lifelong monitoring is essential:
- Serial serum calcium and PTH levels
- Imaging at regular intervals
- Prompt re-operation in case of local recurrence
Recurrence rates can be as high as 50%, often within 3–5 years of initial surgery. Early detection significantly impacts prognosis.
Prognosis and Survival Rates
Prognosis depends on:
- Completeness of the initial resection
- Presence of metastases at diagnosis
- Biochemical control of hypercalcemia
- Histopathological aggressiveness
Five-year survival ranges from 50–85%, but drops significantly in patients with persistent hypercalcemia or inoperable disease.
Recent Advances and Research
- Molecular profiling reveals HRPT2/CDC73 mutations in up to 70% of cases, linked to parafibromin loss
- Genetic testing is recommended for patients with familial hyperparathyroidism or early-onset disease
- Clinical trials are exploring PTH receptor antagonists and immunotherapies as potential adjunct treatments
Frequently Asked Questions
What is parathyroid carcinoma?
A rare malignant tumor of the parathyroid gland causing excessive PTH secretion and life-threatening hypercalcemia.
How is parathyroid carcinoma different from adenoma?
Carcinoma shows invasive growth, recurrence, and severe biochemical imbalance, whereas adenoma is benign and less aggressive.
Can parathyroid carcinoma be cured?
Complete surgical excision offers the best chance for cure. However, recurrence is common and requires ongoing surveillance.
What is the main cause of death in parathyroid carcinoma?
Uncontrolled hypercalcemia leading to renal failure, cardiac arrhythmias, or systemic organ dysfunction is the primary cause.
How is hypercalcemia treated in these patients?
Through hydration, diuretics, bisphosphonates, calcitonin, and surgical resection of the tumor.
Parathyroid carcinoma with hypercalcemia is a medical and surgical emergency requiring timely recognition and multidisciplinary care. Differentiating it from benign causes of primary hyperparathyroidism is critical. While surgery remains the cornerstone of treatment, ongoing advancements in diagnostics and molecular therapy are offering new hope in managing this rare but deadly disease.