Panic disorder is a chronic mental health condition characterized by recurrent, unexpected panic attacks—sudden episodes of intense fear or discomfort that reach a peak within minutes. These episodes are often accompanied by overwhelming physical symptoms and persistent concern about future attacks, leading to significant impairment in daily functioning. The disorder typically emerges in late adolescence or early adulthood and can occur with or without agoraphobia.
Key Features and Diagnostic Criteria
Defining Panic Attacks
A panic attack is defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as an abrupt surge of intense fear or discomfort that peaks within minutes. To meet diagnostic criteria for a panic disorder, individuals must experience:
- Recurrent unexpected panic attacks
- Persistent concern or worry about additional attacks
- Significant behavioral changes related to the attacks
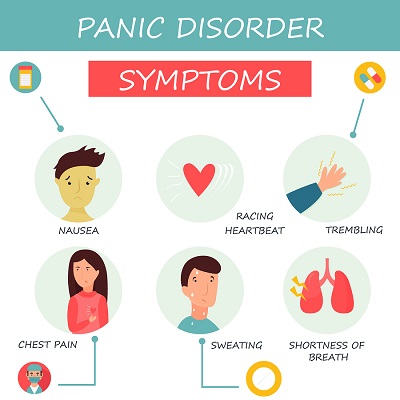
Common Physical and Psychological Symptoms
- Palpitations or accelerated heart rate
- Sweating, trembling, or shaking
- Sensations of shortness of breath or choking
- Chest pain or discomfort
- Nausea or abdominal distress
- Dizziness or lightheadedness
- Derealization or depersonalization
- Fear of losing control or dying
Pathophysiology and Underlying Mechanisms
The exact cause of panic disorder is multifactorial, involving both biological and psychological components. The interplay of genetic predisposition, neurochemical imbalances, and environmental stressors contributes to its onset and progression.
Neurobiological Factors
- Amygdala dysfunction: Hyperactivity in this brain region is associated with heightened fear response.
- Hypothalamic-Pituitary-Adrenal (HPA) axis dysregulation: Chronic stress can dysregulate cortisol production, increasing anxiety sensitivity.
- Neurotransmitter imbalance: Abnormalities in serotonin, norepinephrine, and gamma-aminobutyric acid (GABA) contribute to panic vulnerability.
Risk Factors and Epidemiology
Risk Factors
- Genetics: First-degree relatives are at increased risk
- Major life stressors: Loss, trauma, or major transitions
- Personality traits: Higher neuroticism and sensitivity to stress
- Comorbid mental disorders: Depression, generalized anxiety disorder, substance abuse
Epidemiological Data
- Lifetime prevalence: 2–3% globally
- Gender distribution: More common in females than males
- Onset age: Typically between 20 and 30 years
Differential Diagnosis: Excluding Other Conditions
It is essential to differentiate panic disorder from other medical and psychiatric conditions:
- Cardiac arrhythmias or angina
- Thyroid dysfunction
- Pheochromocytoma
- Substance-induced anxiety
- Post-traumatic stress disorder (PTSD)
- Generalized anxiety disorder (GAD)
Comprehensive evaluation includes physical examination, laboratory testing, and detailed psychiatric assessment to exclude these differentials.
Diagnostic Assessment Tools
Clinical Interview
A structured psychiatric interview based on DSM-5 criteria is the primary method for diagnosing panic disorder.
Standardized Questionnaires
- Panic Disorder Severity Scale (PDSS)
- Hamilton Anxiety Rating Scale (HAM-A)
- Beck Anxiety Inventory (BAI)
These tools assess the frequency, intensity, and impact of panic attacks.
Evidence-Based Treatment Approaches
Cognitive Behavioral Therapy (CBT)
CBT is the first-line psychotherapeutic intervention for panic disorder. It involves:
- Cognitive restructuring to challenge catastrophic thoughts
- Interoceptive exposure to reduce fear of physical sensations
- Behavioral experiments to build resilience
CBT has consistently shown high efficacy in both short- and long-term management.
Pharmacotherapy
Medication may be used alone or in combination with therapy, particularly in moderate to severe cases.
First-line medications:
- Selective serotonin reuptake inhibitors (SSRIs): Sertraline, paroxetine, fluoxetine
- Serotonin-norepinephrine reuptake inhibitors (SNRIs): Venlafaxine
Alternative medications:
- Benzodiazepines: Short-term use for acute episodes (e.g., alprazolam, clonazepam)
- Tricyclic antidepressants: Imipramine, clomipramine
Lifestyle Modifications
- Regular aerobic exercise
- Sleep hygiene improvement
- Limiting caffeine and alcohol
- Mindfulness and relaxation techniques
Prognosis and Long-term Management
The prognosis for panic disorder is generally favorable with appropriate treatment. However, the risk of relapse remains without continued therapeutic engagement.
| Factor | Impact on Prognosis |
|---|---|
| Early intervention | Better outcomes |
| Comorbid depression | Poorer prognosis |
| Medication adherence | Improved symptom control |
| Ongoing stressors | Increased relapse risk |
Periodic reassessment and personalized care plans are essential to sustain remission and ensure functional recovery.
Complications and Associated Conditions
If left untreated, panic disorder can lead to:
- Agoraphobia: Avoidance of places where escape might be difficult
- Substance abuse: Often used to self-medicate symptoms
- Major depressive disorder
- Occupational and social impairment
Proactive treatment significantly reduces these risks and enhances quality of life.
Frequently Asked Questions
What triggers a panic attack?
Triggers may include stress, certain environments, physical sensations, or may occur spontaneously with no identifiable cause.
Can panic disorder be cured?
While a permanent “cure” may not apply to all individuals, many achieve complete remission with therapy and medication.
How long does a panic attack last?
Most panic attacks peak within 10 minutes and resolve within 30 minutes, though residual symptoms can linger.
Is medication always necessary?
Not always. Mild to moderate cases often respond well to CBT alone. Medications are helpful in more severe or persistent cases.
Can panic disorder lead to other mental health conditions?
Yes, particularly depression, agoraphobia, and substance use disorders if untreated.

