Ovarian follicle maturation induction refers to the deliberate medical stimulation of the ovaries to promote the growth and development of ovarian follicles, culminating in ovulation. This technique plays a vital role in treating anovulation, oligo-ovulation, and in assisted reproductive technologies (ART), especially in in vitro fertilization (IVF) protocols. Through the use of exogenous hormones, clinicians can manipulate the natural hormonal environment to achieve controlled follicular development and ovulation at a precise time.
Physiology of Follicular Development and Maturation
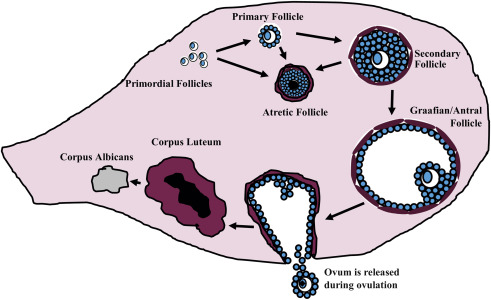
Ovarian folliculogenesis progresses through several well-defined stages under the influence of gonadotropins:
Hormonal Regulation:
- Follicle-Stimulating Hormone (FSH): Stimulates granulosa cell proliferation and aromatase activity.
- Luteinizing Hormone (LH): Triggers the final maturation and ovulation.
- Estradiol (E2): Produced by granulosa cells; provides feedback on the hypothalamus and pituitary.
- Inhibin B and A: Regulate FSH secretion.
During a natural cycle, a cohort of antral follicles becomes sensitive to FSH, but only one becomes dominant, suppressing others via estradiol and inhibin. In induction protocols, this natural selection is overridden to recruit multiple follicles.
Indications for Follicle Maturation Induction
1. Anovulatory or Oligo-ovulatory Infertility
- Polycystic Ovary Syndrome (PCOS): Most common cause of chronic anovulation.
- Hypothalamic amenorrhea
- Luteal phase defects
2. Controlled Ovarian Stimulation in ART
- IVF and intrauterine insemination (IUI) protocols often require synchronized multi-follicular development to maximize success.
3. Poor Ovarian Reserve
- Women with low anti-Müllerian hormone (AMH) or advanced reproductive age benefit from stimulation to optimize the response.
Protocols for Ovarian Follicle Maturation Induction
Clomiphene Citrate (CC) Protocol
- Mechanism: Selective estrogen receptor modulator (SERM) that blocks estrogen receptors in the hypothalamus.
- Effect: Increases endogenous FSH and LH secretion.
- Typical Dose: 50–150 mg/day for 5 days starting on day 2–5 of the menstrual cycle.
Letrozole Protocol
- Mechanism: Aromatase inhibitor reducing estrogen synthesis.
- Effect: Lifts negative feedback on the hypothalamus, enhancing FSH.
- Preferred in: PCOS, due to lower risk of multiple gestations and better endometrial response.
Gonadotropin Protocol
- Medications Used: Recombinant FSH (rFSH), human menopausal gonadotropin (hMG).
- Dosing: Tailored to ovarian reserve and BMI; requires daily injections and close monitoring.
GnRH Analogues
Used to prevent premature LH surge during gonadotropin stimulation.
| Type | Purpose | Timing |
|---|---|---|
| GnRH Agonist | Downregulation of pituitary | Long protocol |
| GnRH Antagonist | Immediate suppression | Short protocol |
Monitoring and Assessment of Follicular Growth
Ultrasound Monitoring
- Follicular Size Tracking: Transvaginal ultrasound every 2–3 days.
- Mature Follicle Criteria: Diameter of 17–20 mm.
Hormonal Monitoring
- Estradiol Levels: Correlates with follicular maturity.
- LH and Progesterone: Monitored to prevent premature ovulation.
Ovulation Trigger and Timing
Ovulation is induced when the lead follicles reach adequate size and estradiol levels peak.
Common Triggers:
- hCG Injection (10,000 IU): Mimics LH surge, leading to ovulation in 36–40 hours.
- GnRH Agonist Trigger: Used in antagonist cycles to reduce ovarian hyperstimulation syndrome (OHSS) risk.
Post-Induction Strategies
1. Timed Intercourse or Insemination
- Planned around 36 hours post-trigger.
2. Oocyte Retrieval for IVF
- Performed just before natural ovulation (~34–36 hours post-trigger).
3. Luteal Phase Support
- Progesterone supplementation is often administered following ovulation to support implantation.
Risks and Complications
Ovarian Hyperstimulation Syndrome (OHSS)
- Potentially life-threatening complication marked by enlarged ovaries and fluid shift.
- More common in high responders, especially with hCG trigger.
Multiple Pregnancy
- Especially with gonadotropin and CC protocols.
- Letrozole has lower associated risk.
Cycle Cancellation
- Inadequate response or over-response (too many follicles) may lead to cycle termination to avoid complications.
Optimizing Success in Follicle Maturation Induction
- Individualized Protocols: Based on age, BMI, AMH, antral follicle count.
- Frequent Monitoring: Essential for adjusting doses and avoiding complications.
- Adjunctive Therapies: Use of insulin sensitizers (e.g., metformin) in PCOS to improve response.
Frequently Asked Questions:
How long does ovarian follicle maturation induction take?
Typically, 10–14 days from the start of stimulation to ovulation.
Can follicle induction help all types of infertility?
It is effective primarily in cases related to ovulatory dysfunction and is central to ART cycles.
What is the ideal number of follicles for IVF retrieval?
Between 8–15 mature follicles are considered optimal for high success and low OHSS risk.
Is it painful to undergo ovarian stimulation?
Mild discomfort or bloating is common; pain is usually minimal.
Can follicular maturation induction fail?
Yes. Poor responders or women with diminished ovarian reserve may require multiple cycles or alternative approaches.
Ovarian follicle maturation induction stands as a cornerstone in modern fertility management, offering women with ovulatory dysfunction or those undergoing ART the chance to conceive through medically guided ovarian stimulation. By employing targeted hormonal protocols and personalized care, clinicians can effectively manage follicular development, optimize ovulation timing, and improve pregnancy outcomes. Continued advancements in monitoring and pharmacologic agents promise to further refine and enhance this critical reproductive intervention.