Osteomyelitis is a serious infection of the bone characterized by inflammation, necrosis, and new bone formation. It can result from hematogenous spread, direct inoculation from trauma or surgery, or contiguous spread from nearby infections. Prompt recognition and aggressive management are crucial to prevent chronic complications, bone destruction, or systemic involvement.
Pathophysiology of Osteomyelitis
Osteomyelitis occurs when pathogens, most commonly Staphylococcus aureus, invade bone tissue. Bacterial colonization initiates an inflammatory response leading to increased intramedullary pressure, vascular compromise, and eventual bone necrosis. In chronic cases, dead bone (sequestrum) forms, surrounded by reactive new bone (involucrum), complicating treatment.
Types of Osteomyelitis
1. Acute Osteomyelitis
- Rapid onset, often within days.
- More common in children.
- Typically caused by hematogenous spread.
2. Chronic Osteomyelitis
- Develops over weeks or months.
- Often follows inadequate treatment of acute infection or post-trauma.
- Characterized by persistent infection and necrotic bone.
3. Vertebral Osteomyelitis
- Frequently seen in older adults.
- Hematogenous spread affecting vertebral bodies.
- Commonly caused by Staphylococcus aureus, E. coli, and Mycobacterium tuberculosis.
4. Contiguous-Focus Osteomyelitis
- Resulting from nearby soft tissue infection or open fracture.
- Common in diabetic foot ulcers and pressure sores.
5. Osteomyelitis Related to Vascular Insufficiency
- Typically seen in diabetic patients.
- Poor perfusion impairs immune response and healing.
Common Causes and Risk Factors
- Hematogenous Spread: From bacteremia in children or elderly.
- Direct Inoculation: Following fractures, orthopedic surgeries, or penetrating wounds.
- Contiguous Spread: Skin infections, cellulitis, or infected prosthetic joints.
- Immunocompromised States: Diabetes, HIV, malignancy, corticosteroid therapy.
- Peripheral Vascular Disease: Leads to poor circulation and delayed healing.
Clinical Presentation of Osteomyelitis
General Symptoms
- Fever and chills
- Malaise
- Localized pain and tenderness
- Swelling and erythema over the affected area
- Restricted movement of nearby joints
Chronic Osteomyelitis Indicators
- Sinus tract formation
- Recurrent infection
- Purulent discharge
- Non-healing ulcers (especially in diabetics)
Diagnostic Approach
Accurate diagnosis involves a combination of clinical assessment, imaging studies, and microbiological analysis.
Laboratory Investigations
| Test | Typical Finding |
|---|---|
| White Blood Cell Count (WBC) | Elevated in acute cases |
| ESR (Erythrocyte Sedimentation Rate) | Markedly elevated |
| CRP (C-reactive protein) | Elevated, useful for monitoring |
| Blood Cultures | Positive in hematogenous spread |
| Culture and Sensitivity | Identifies pathogen from aspirates or bone biopsy |
Imaging Modalities
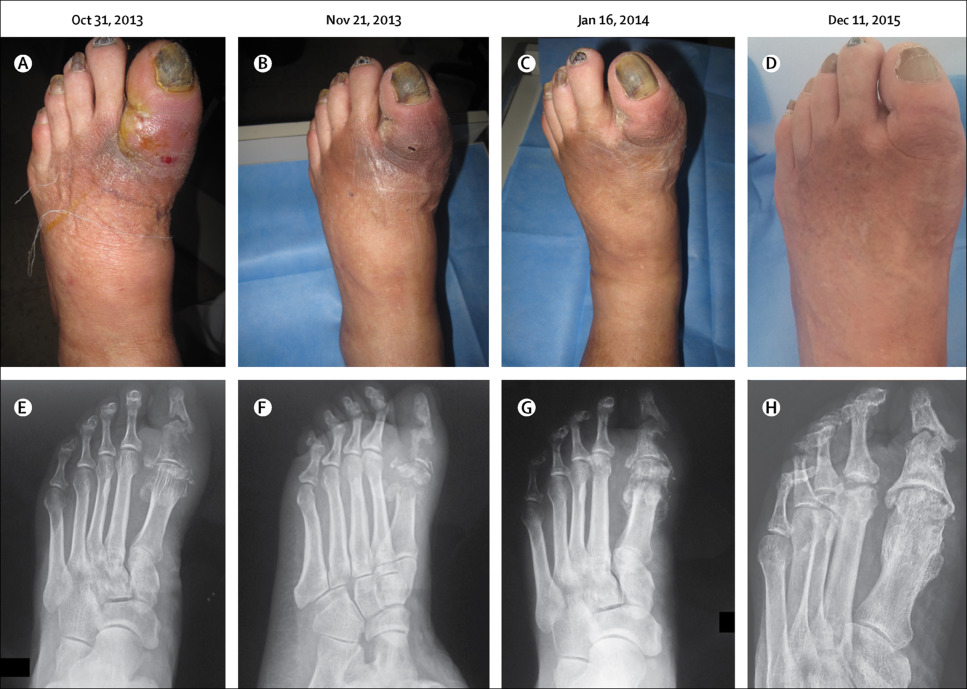
- X-rays: May show bone destruction, periosteal reaction in late stages.
- MRI: Most sensitive early diagnostic tool. Shows marrow edema and abscesses.
- CT Scan: Detects sequestra and cortical destruction.
- Radionuclide Bone Scan: Useful when MRI is contraindicated.
- PET Scan: High sensitivity for chronic osteomyelitis.
- Bone Biopsy: Gold standard for definitive diagnosis and pathogen identification.
Classification Systems
Cierny-Mader Classification
| Type | Description |
|---|---|
| Type I | Medullary infection |
| Type II | Superficial infection |
| Type III | Localized full-thickness infection |
| Type IV | Diffuse osteomyelitis |
This system also classifies the host as:
- A (healthy),
- B (compromised),
- C (poor surgical candidate).
Treatment of Osteomyelitis
Management depends on disease acuity, pathogen, anatomical site, and host status.
Medical Management
- Empirical Antibiotics: Initiated after cultures; commonly cover Staphylococcus aureus, including MRSA.
- Targeted Antibiotics: Adjusted based on culture sensitivity. Duration: 4–6 weeks IV or oral based on severity.
- Adjunct Therapies: Pain management, antipyretics, nutritional support.
Surgical Management
- Debridement: Removal of necrotic bone and infected tissue.
- Sequestrectomy: Extraction of sequestrum in chronic cases.
- Stabilization: External or internal fixation in case of pathological fractures.
- Soft Tissue Coverage: Use of muscle or skin flaps in case of large defects.
- Amputation: Last resort in non-salvageable limbs with systemic sepsis.
Modern Interventions
- Local Antibiotic Delivery: Antibiotic-impregnated beads or cement spacers.
- Negative Pressure Wound Therapy (NPWT): Enhances wound healing.
- Hyperbaric Oxygen Therapy (HBOT): Facilitates oxygenation and neovascularization in chronic infections.
Prevention Strategies
- Sterile Surgical Technique: Especially in orthopedic procedures.
- Early Management of Wounds: Proper wound care in trauma and diabetic ulcers.
- Glycemic Control: Essential for diabetic patients.
- Prophylactic Antibiotics: In high-risk surgical cases.
- Patient Education: Awareness about foot care, hygiene, and early signs of infection.
Prognosis and Long-Term Outlook
Prompt diagnosis and effective treatment result in excellent outcomes for acute osteomyelitis. However, chronic osteomyelitis may require multiple interventions, and recurrence is possible. Long-term disability, reduced limb function, and amputations are risks in advanced or poorly managed cases.
Frequently Asked Questions
What is osteomyelitis?
Osteomyelitis is an infection in the bone, commonly caused by bacteria and resulting in inflammation and bone destruction.
Is osteomyelitis a life-threatening condition?
If untreated, it can lead to chronic infection, sepsis, or even death, especially in immunocompromised patients.
How long does it take to recover from osteomyelitis?
Recovery depends on severity but typically requires 4–6 weeks of antibiotics and possibly surgery.
Can osteomyelitis recur after treatment?
Yes, especially if not fully treated or in cases with underlying risk factors like diabetes.
Can osteomyelitis spread to other parts of the body?
Yes, through the bloodstream, it can lead to systemic infection (sepsis) or affect adjacent joints.
Osteomyelitis remains a challenging clinical entity due to its varied presentation and potential for chronicity. Early recognition, comprehensive diagnosis, and a multidisciplinary treatment approach are key to successful outcomes. With advances in imaging, antimicrobial therapy, and surgical techniques, even complex cases can be managed effectively, improving patient quality of life and limb function.