Osteoarthritis (OA) is the most prevalent form of arthritis, characterized by the gradual degradation of articular cartilage and underlying bone in synovial joints. It is a progressive, chronic joint disorder that primarily affects the knees, hips, hands, and spine. The condition results in pain, stiffness, reduced function, and a significant decline in quality of life.
Osteoarthritis affects over 300 million people worldwide and is a leading cause of disability in older adults. While traditionally considered a “wear and tear” disease, current understanding recognizes the complex interplay of mechanical, genetic, metabolic, and inflammatory factors.
Pathophysiology: Understanding Joint Degeneration
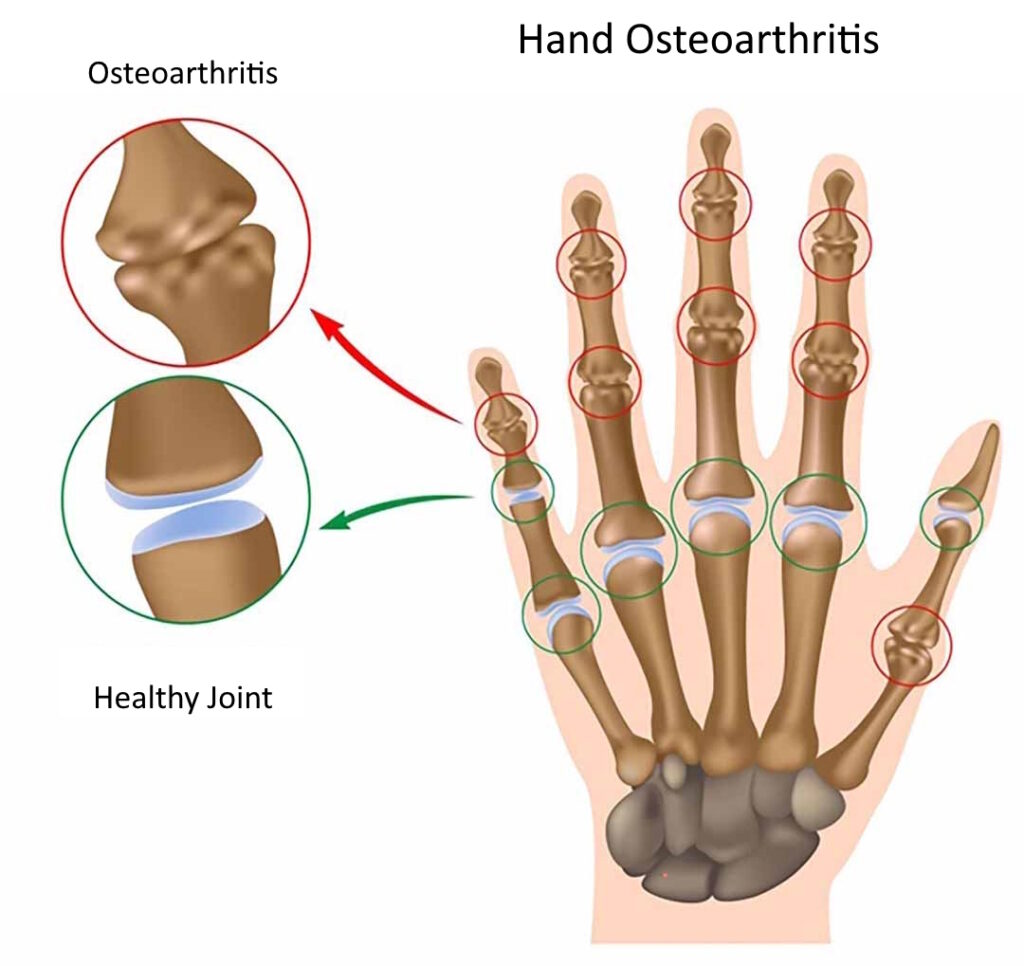
The hallmark of osteoarthritis is cartilage degradation. Articular cartilage acts as a smooth, lubricated surface that facilitates joint movement and absorbs shock. In OA, the cartilage becomes rough and thins, leading to increased friction, bone remodeling, and inflammation.
Additional changes include:
- Synovial inflammation
- Subchondral bone sclerosis
- Meniscal degeneration
- Ligamentous laxity
Common Causes and Risk Factors
Osteoarthritis results from a combination of intrinsic and extrinsic factors that disrupt joint homeostasis.
Major Risk Factors:
- Age: Incidence increases significantly after 50
- Genetics: Family history influences susceptibility
- Gender: More common and severe in women
- Obesity: Increases joint load and promotes inflammation
- Joint injury: Trauma or repetitive stress accelerates degeneration
- Occupation: Jobs involving heavy lifting, kneeling, or squatting
- Joint malalignment: Alters load distribution within joints
Clinical Presentation: Symptoms of Osteoarthritis
The symptoms of osteoarthritis typically develop slowly and worsen over time.
Key Symptoms:
- Joint pain: Worsens with activity, relieved by rest
- Stiffness: Especially after periods of inactivity or in the morning (<30 minutes)
- Swelling: Due to synovial inflammation
- Decreased range of motion
- Joint crepitus: Grating sensation with movement
- Joint deformity: In advanced stages
Affected joints often include:
- Knees
- Hips
- Hands (distal and proximal interphalangeal joints, first carpometacarpal joint)
- Spine (cervical and lumbar regions)
Diagnosis: Clinical and Imaging Evaluation
Osteoarthritis is primarily diagnosed through clinical evaluation, supported by imaging and, occasionally, laboratory studies.
Clinical Criteria (ACR Guidelines):
- Persistent joint pain
- Morning stiffness under 30 minutes
- Crepitus on motion
- Bony tenderness or enlargement
Imaging Studies:
- X-rays: Joint space narrowing, osteophytes, subchondral sclerosis, cysts
- MRI: Detailed assessment of cartilage and soft tissue structures
- Ultrasound: Synovial inflammation, effusion
Laboratory Tests:
- Typically used to rule out inflammatory arthropathies
- ESR, CRP: Usually normal
- Synovial fluid analysis: Non-inflammatory in OA
Staging and Grading Severity
The Kellgren-Lawrence grading system is widely used to assess radiographic severity:
| Grade | Description |
|---|---|
| 0 | No radiographic features of OA |
| 1 | Doubtful narrowing of joint space |
| 2 | Definite osteophytes, possible narrowing |
| 3 | Moderate narrowing, multiple osteophytes |
| 4 | Severe narrowing, large osteophytes, bone deformity |
Treatment Options for Osteoarthritis
Management is focused on relieving symptoms, improving function, and slowing disease progression. A combination of non-pharmacological and pharmacological interventions is recommended.
Non-Pharmacologic Therapies
- Weight loss: Reduces mechanical stress on weight-bearing joints
- Exercise: Strengthening, aerobic, and flexibility training
- Physical therapy: Gait training, balance improvement
- Assistive devices: Braces, orthotics, canes
- Occupational therapy: Joint protection techniques
Pharmacologic Treatments
- Acetaminophen: First-line for mild pain
- NSAIDs: Ibuprofen, naproxen, diclofenac for inflammation and pain
- Topical agents: Capsaicin, NSAID gels
- Intra-articular injections:
- Corticosteroids: Short-term relief of inflammation
- Hyaluronic acid: Viscosupplementation with mixed evidence
- Duloxetine: For chronic pain management
Surgical Intervention
Indicated for patients with severe symptoms and structural joint damage unresponsive to conservative measures.
- Arthroscopy: Debridement (limited benefit)
- Osteotomy: Realignment for joint preservation
- Joint replacement (arthroplasty):
- Total knee or hip replacement
- Long-term relief and functional improvement
Lifestyle Modifications and Long-Term Management
Long-term osteoarthritis management relies heavily on patient education and lifestyle adaptation.
Key Strategies:
- Maintaining ideal body weight
- Adopting a joint-friendly fitness routine
- Avoiding high-impact activities
- Using ergonomic aids in daily activities
- Regular monitoring to adjust treatments
Future Directions in Osteoarthritis Research
Emerging therapies target the underlying pathophysiology, aiming to modify disease progression.
Promising Areas:
- Biologic therapies: Inhibiting inflammatory cytokines like IL-1 and TNF-α
- Gene therapy: Promoting cartilage regeneration
- Tissue engineering: Stem cells and 3D-printed cartilage
- Novel biomarkers: Early detection and personalized therapy
Frequently Asked Questions:
Is osteoarthritis the same as arthritis?
Osteoarthritis is a specific type of arthritis caused by cartilage degeneration. It differs from inflammatory types such as rheumatoid arthritis.
Can osteoarthritis be cured?
There is no cure, but symptoms can be effectively managed with lifestyle changes, medications, and in severe cases, surgery.
What foods help with osteoarthritis?
Anti-inflammatory diets rich in omega-3 fatty acids, antioxidants, and whole grains may help reduce symptoms.
Is walking good for osteoarthritis?
Yes, regular low-impact exercise like walking strengthens muscles and maintains joint flexibility.
Can weather affect osteoarthritis symptoms?
Many patients report increased pain with cold or damp weather, though the exact mechanisms are not fully understood.
Osteoarthritis is a complex and multifactorial condition with a growing global burden. Effective management requires a holistic and individualized approach, combining lifestyle modifications, evidence-based medical therapy, and, when necessary, surgical intervention. Ongoing advancements in research continue to offer hope for disease-modifying strategies that may transform osteoarthritis care in the near future.