Organophos Insecticide Poisoning: Organophosphate (organophos) insecticides are widely used agricultural chemicals that pose serious risks to human health upon exposure. Poisoning typically results from accidental ingestion, occupational exposure, or intentional self-harm and can lead to life-threatening cholinergic toxicity due to the inhibition of acetylcholinesterase, a critical enzyme in the nervous system.
Organophos insecticide poisoning is a medical emergency that demands rapid recognition, accurate diagnosis, and aggressive treatment to prevent morbidity and mortality.
Mechanism of Toxicity: Acetylcholinesterase Inhibition
Organophosphates exert their toxic effects by irreversibly inhibiting acetylcholinesterase (AChE), leading to the accumulation of acetylcholine (ACh) at synaptic junctions. This overstimulation of cholinergic receptors causes both muscarinic and nicotinic symptoms, as well as central nervous system (CNS) manifestations.
Common Sources of Exposure
- Agricultural applications (e.g., spraying of crops)
- Improper storage or handling of insecticides
- Household pesticide use
- Contaminated food or water
- Suicidal ingestion, particularly in rural areas
Widely used organophosphates include malathion, chlorpyrifos, diazinon, parathion, and phorate.
Clinical Presentation of Organophos Poisoning
The symptomatology of organophosphate poisoning reflects widespread cholinergic overstimulation.
Muscarinic Symptoms
- Salivation
- Lacrimation
- Urination
- Diarrhea
- Gastrointestinal cramps
- Emesis
(Mnemonic: SLUDGE) - Miosis (pinpoint pupils)
- Bronchorrhea, bronchospasm
- Bradycardia, hypotension
Nicotinic Symptoms
- Muscle fasciculations
- Cramps
- Paralysis
- Tachycardia
- Hypertension
CNS Symptoms
- Anxiety, confusion
- Seizures
- Coma
- Respiratory failure
Diagnosis of Organophosphate Toxicity
Clinical Assessment
Diagnosis is primarily clinical, based on the patient’s symptoms, history of exposure, and characteristic odor of organophosphates (garlic or petroleum-like).
Laboratory Investigations
- Red Blood Cell Acetylcholinesterase (RBC AChE): More specific and correlates with neurological symptoms.
- Plasma pseudocholinesterase (butyrylcholinesterase): Easier to test but less specific.
- Arterial blood gases (ABG): To assess respiratory status and acidosis
- Electrolytes, renal and liver function tests
- Chest X-ray: For aspiration pneumonia or pulmonary edema
Prompt measurement of enzyme activity is critical to assess the severity and monitor therapeutic response.
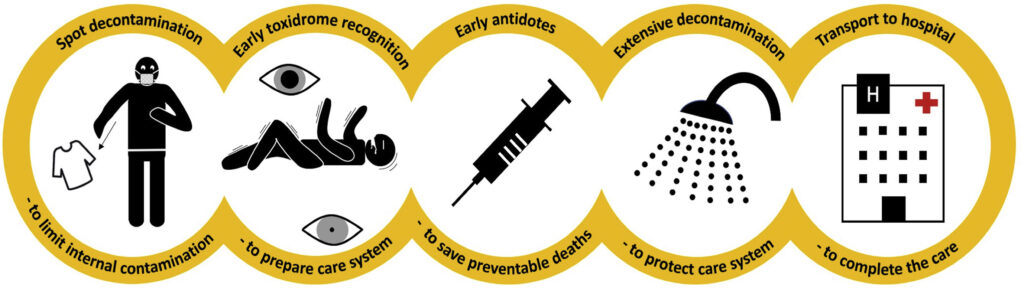
Management and Treatment of Organophos Insecticide Poisoning
Decontamination
- Remove contaminated clothing
- Irrigate skin and mucous membranes thoroughly with water
- Activated charcoal if ingestion occurred within one hour
Airway Management
- Ensure a patent airway
- Administer oxygen
- Prepare for intubation in patients with altered mental status or respiratory failure
Antidotal Therapy
Atropine
- Mechanism: Competitive antagonist at muscarinic receptors
- Dose: 1–2 mg IV every 5–10 minutes, doubled until bronchial secretions are cleared and heart rate stabilizes
- End Point: Dry lungs, adequate oxygenation, stable vitals
Oximes (e.g., Pralidoxime)
- Mechanism: Reactivates AChE by removing the phosphate group
- Dose: 30 mg/kg IV over 30 minutes, followed by continuous infusion
- Effective for: Nicotinic symptoms, muscle weakness, and fasciculations
Supportive Care
- Benzodiazepines (e.g., diazepam) for seizures
- IV fluids for hypotension
- Mechanical ventilation if respiratory failure develops
- Monitoring in ICU with frequent vital signs, AChE levels
Intermediate Syndrome and Delayed Neuropathy
Intermediate Syndrome
Occurs 24–96 hours post-exposure:
- Proximal muscle weakness
- Cranial nerve palsies
- Respiratory insufficiency
- Requires prolonged mechanical ventilation
Organophosphate-Induced Delayed Neuropathy (OPIDN)
- Appears 1–3 weeks after exposure
- Sensory-motor peripheral neuropathy
- Lower limb weakness
- No effective treatment; rehabilitation is key
Prognosis and Mortality
- Mortality rate: 10–40%, depending on dose, time to treatment, and availability of intensive care
- Complications: Respiratory failure, arrhythmias, aspiration pneumonia, prolonged ICU stay
- Better outcomes with early recognition, rapid atropinization, and ICU support
Prevention Strategies and Public Health Importance
Safety Measures
- Personal protective equipment (PPE) for agricultural workers
- Proper storage and labeling of pesticides
- Regulation and restriction of highly toxic OP compounds
- Public education on the dangers of improper pesticide use
Policy-Level Interventions
- Banning of high-risk organophosphates in many countries
- Introduction of Integrated Pest Management (IPM) to reduce reliance on chemical pesticides
Frequently Asked Questions:
What is the first-line treatment for organophosphate poisoning?
Atropine is the primary antidote, used to counteract muscarinic symptoms.
How is pralidoxime different from atropine?
Pralidoxime reverses the cause by reactivating acetylcholinesterase, whereas atropine only treats symptoms.
Can organophosphate poisoning be delayed in onset?
Yes. Intermediate syndrome and delayed neuropathy can occur days or weeks after initial exposure.
Is vomiting a reliable indicator of poisoning severity?
Not necessarily. Severity is better assessed by respiratory distress, level of consciousness, and enzyme activity.
What should be done after skin exposure to insecticides?
Immediate removal of clothing and thorough irrigation with water is essential.
Organophos insecticide poisoning is a medical and public health concern that demands urgent clinical attention. Characterized by its profound cholinergic effects, timely diagnosis and aggressive intervention with atropine, oximes, and supportive care are crucial for survival. Prevention through education, regulation, and protective measures is equally vital to reduce incidence and improve outcomes across vulnerable populations.