Beta-blockers are a class of medications widely prescribed to manage cardiovascular conditions such as hypertension, arrhythmias, and heart failure. Although these drugs are effective in treating such conditions, the risk of overdose poses a serious health concern. In this article, we will explore the symptoms of a beta-blocker overdose, its causes, available treatment options, and how to manage the condition to ensure optimal recovery and prevent long-term complications.
What Are Beta-Blockers?
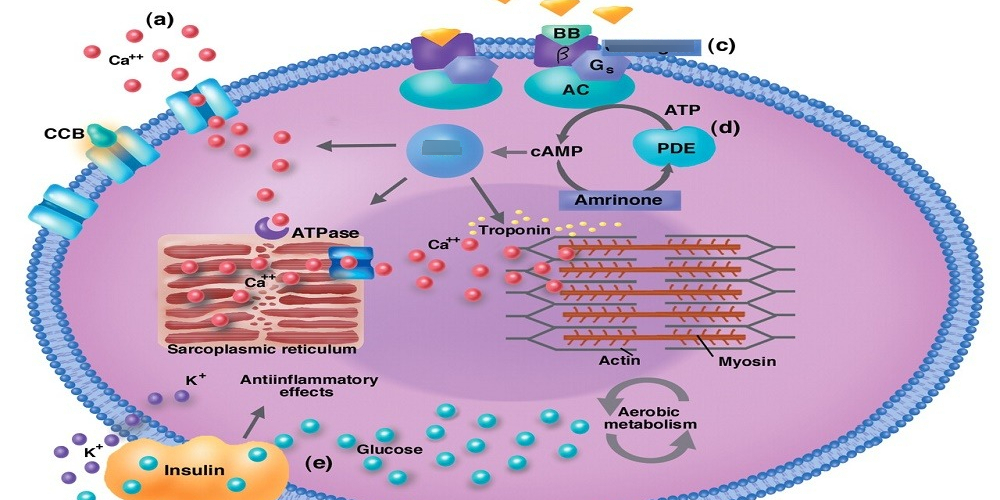
Beta-blockers, also known as beta-adrenergic blockers, are medications that block the effects of adrenaline (epinephrine) on the beta receptors of the heart and blood vessels. By doing so, they lower heart rate, reduce blood pressure, and prevent abnormal heart rhythms. Common beta-blockers include:
- Atenolol
- Metoprolol
- Propranolol
- Carvedilol
- Bisoprolol
These medications are frequently used in treating conditions such as high blood pressure, chronic heart failure, and anxiety. Despite their therapeutic benefits, beta-blockers can become dangerous when consumed in excessive quantities.
Symptoms of Beta-Blocker Overdose
An overdose of beta-blockers can be life-threatening if not promptly addressed. Symptoms typically depend on the severity of the overdose and can affect various body systems, particularly the cardiovascular system. Key symptoms of a beta-blocker overdose include:
- Bradycardia (Slow Heart Rate): One of the hallmark signs of an overdose is a heart rate significantly lower than normal, often under 60 beats per minute.
- Hypotension (Low Blood Pressure): Overdose can cause a drastic drop in blood pressure, leading to dizziness, fainting, or shock.
- Respiratory Depression: Difficulty breathing, labored respiration, or even respiratory arrest may occur in severe cases.
- Fatigue and Weakness: Excessive beta-blockade can lead to extreme tiredness and muscle weakness.
- Hypoglycemia (Low Blood Sugar): In some cases, beta-blocker overdose can impair the body’s ability to regulate blood sugar levels.
- Confusion or Dizziness: Decreased blood flow to the brain may result in cognitive impairment and a general sense of confusion.
- Severe Heart Block or Cardiac Arrest: In critical overdoses, electrical conduction within the heart can become severely impaired, potentially leading to a heart attack or death.
Causes of Beta-Blocker Overdose
The primary cause of a beta-blocker overdose is the consumption of more than the prescribed dose. Overdose scenarios can happen accidentally or intentionally. Common contributing factors include:
- Accidental Overdose: Individuals may mistakenly take an extra dose of their medication, or children may ingest a family member’s medication.
- Intentional Overdose: In some cases, individuals may overdose as a result of suicide attempts or self-harm. This is particularly concerning with patients who have underlying mental health conditions.
- Drug Interactions: The combination of beta-blockers with certain medications, such as calcium channel blockers, can amplify the risk of overdose.
- Alcohol Use: Alcohol may exacerbate the effects of beta-blockers, leading to dangerous side effects when taken together in high amounts.
Treatment for Beta-Blocker Overdose
Immediate medical intervention is crucial for individuals suspected of overdosing on beta-blockers. Treatment strategies depend on the severity of the overdose and the symptoms presented. Standard treatment options include:
1. Activated Charcoal
Activated charcoal may be administered in cases of recent ingestion (typically within one hour) to prevent further absorption of the drug from the stomach. This is particularly effective if the overdose is confirmed shortly after ingestion.
2. Intravenous Fluids
IV fluids are often administered to combat hypotension and help stabilize the patient’s blood pressure. This treatment is essential in preventing organ failure due to low blood flow.
3. Atropine
For patients experiencing severe bradycardia or heart block, atropine, a medication that stimulates the heart, may be given. Atropine works by increasing the heart rate, counteracting the slowing effects of the beta-blockers.
4. Glucagon
Glucagon is a hormone that can be administered intravenously to increase heart rate and blood pressure in patients suffering from beta-blocker overdose. It can help restore normal cardiovascular function and act as an antidote to the overdose.
5. Pacemaker Therapy
In cases of severe heart block, a temporary pacemaker may be necessary to regulate the heart’s electrical activity and prevent cardiac arrest.
6. Lipid Emulsion Therapy
In severe overdoses, lipid emulsion therapy may be used. This treatment involves infusing fat-based fluids that help bind and remove the excess beta-blocker from the bloodstream.
7. Supportive Care
Patients may require prolonged monitoring in a hospital setting. Supportive care may include supplemental oxygen, mechanical ventilation, and continuous monitoring of vital signs such as heart rate and blood pressure.
How to Manage and Prevent Beta-Blocker Overdose
Prevention of beta-blocker overdose largely centers around careful management of prescribed doses and adherence to safety guidelines:
- Strict Adherence to Prescriptions: Patients should follow the prescribed dosage instructions closely and never adjust the dose without consulting a healthcare professional.
- Proper Storage: Beta-blockers should be kept in a secure location to prevent accidental ingestion, especially by children.
- Awareness of Drug Interactions: Individuals should inform their healthcare provider about all medications they are taking, including over-the-counter drugs, supplements, and alcohol, to avoid dangerous interactions.
- Mental Health Support: People with mental health conditions or those at risk of self-harm should receive appropriate counseling and care to reduce the risk of intentional overdose.