Opioid-induced constipation (OIC) is one of the most prevalent and distressing adverse effects of opioid therapy. Unlike other opioid side effects such as sedation or nausea that may diminish with time, OIC tends to persist throughout treatment and often worsens. It significantly affects patients’ quality of life, treatment adherence, and clinical outcomes, particularly in individuals on chronic pain management or palliative care.
How Opioids Cause Constipation
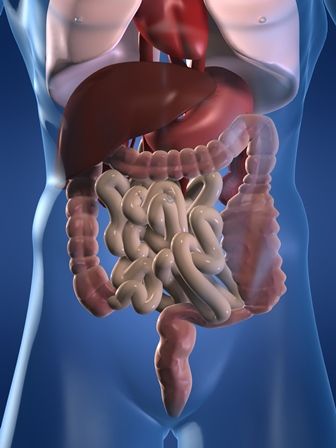
Opioids bind to mu-opioid receptors located not only in the central nervous system (to control pain) but also in the gastrointestinal (GI) tract. Within the GI tract, these receptors modulate several essential processes involved in bowel function.
Mechanisms Involved:
- Reduced intestinal motility
- Delayed gastric emptying
- Increased fluid absorption from stool
- Inhibited secretions from intestinal glands
These effects result in harder stools, infrequent bowel movements, straining, and a constant feeling of incomplete evacuation.
Recognizing the Symptoms of OIC
OIC is not simply occasional constipation. It presents a distinct clinical picture, especially in patients with no prior bowel issues before opioid therapy.
Common Symptoms:
- Fewer than three bowel movements per week
- Hard, dry stools
- Straining during defecation
- Incomplete evacuation sensation
- Bloating and abdominal discomfort
- Early satiety or loss of appetite
Symptoms typically appear within days to weeks of initiating opioid therapy.
Risk Factors for Developing OIC
Several patient-specific and treatment-related factors influence the likelihood and severity of OIC:
- High opioid doses or long-acting formulations
- Concurrent use of anticholinergics or calcium channel blockers
- Poor fluid or fiber intake
- Advanced age
- Immobility or sedentary lifestyle
- Pre-existing GI disorders such as IBS or slow transit colon
Recognizing these risk factors early can inform proactive management strategies.
Differentiating OIC from Functional Constipation
While symptoms may overlap, it is critical to distinguish opioid-induced constipation from functional constipation to ensure targeted treatment.
| Criteria | Opioid-Induced Constipation | Functional Constipation |
|---|---|---|
| Onset | After opioid initiation | May begin at any time |
| Pathophysiology | Mu-opioid receptor effects | Multifactorial, idiopathic |
| Response to laxatives | Often poor | Variable response |
| Management | May require opioid antagonists | Lifestyle and dietary changes |
Strategies for Managing Opioid-Induced Constipation
Stepwise Approach to OIC Treatment
Management of OIC involves a tiered strategy, starting with lifestyle measures and progressing to pharmacological interventions when necessary.
1. Lifestyle and Dietary Adjustments
- Increased water intake (1.5–2L/day)
- High-fiber diet (20–35g/day)
- Regular physical activity
- Establishing a bowel routine
These measures alone are often insufficient in opioid users but should still be encouraged.
2. Traditional Laxatives
First-line pharmacologic agents, though limited in effectiveness for OIC.
- Osmotic laxatives: polyethylene glycol, lactulose
- Stimulant laxatives: senna, bisacodyl
- Stool softeners: docusate sodium
While commonly used, these agents do not address the underlying opioid receptor-mediated mechanism, leading to frequent dissatisfaction.
3. Peripherally Acting Mu-Opioid Receptor Antagonists (PAMORAs)
Target the GI-specific opioid receptors without affecting pain relief.
- Methylnaltrexone (Relistor)
- Naloxegol (Movantik)
- Naldemedine (Symproic)
These agents provide targeted reversal of OIC and are recommended when laxatives fail.
4. Prosecretory Agents
Enhance intestinal fluid secretion and motility.
- Lubiprostone (Amitiza): chloride channel activator
- Linaclotide and Plecanatide: guanylate cyclase-C agonists
These are alternative or adjunctive therapies, particularly in refractory cases.
Preventing OIC Before It Starts
Prophylactic Measures with Opioid Initiation
- Initiate a bowel regimen concurrently with opioid therapy
- Start with an osmotic laxative plus a stimulant
- Educate patients on early symptom recognition
- Regularly monitor bowel function during treatment
Taking a proactive approach helps avoid severe complications like fecal impaction, rectal bleeding, or opioid discontinuation due to intolerable side effects.
OIC in Special Populations
Cancer and Palliative Care Patients
Constipation in these patients is often multifactorial. OIC management should balance comfort and efficacy.
- Methylnaltrexone is particularly effective in palliative care settings, showing rapid onset of action.
- Non-oral routes (subcutaneous injections) may be necessary in advanced disease.
Elderly Patients
Older adults are more susceptible due to physiological slowdowns and polypharmacy. Lower doses and careful titration are essential.
Children and Adolescents
OIC in pediatric patients requires weight-adjusted dosing and careful selection of agents, particularly avoiding stimulant overuse.
Emerging Therapies and Future Directions
Research is ongoing to develop better agents that prevent or reverse OIC without compromising analgesia.
- Combination formulations of opioids with PAMORAs (e.g., oxycodone/naloxone)
- Novel receptor modulators that spare GI motility
- Microbiome-based therapies targeting gut flora affected by opioids
Personalized treatment algorithms based on genetic and metabolic profiles may also become standard in the near future.
Frequently Asked Questions
Q1: How soon does opioid-induced constipation occur?
OIC can develop within the first few days of opioid use, particularly with high doses or long-acting agents.
Q2: Can opioid-induced constipation go away on its own?
Unlikely. OIC persists as long as the opioid is continued and requires active management.
Q3: Do PAMORAs affect pain relief?
No. These medications work peripherally and do not cross the blood-brain barrier, preserving analgesia.
Q4: Is it safe to use laxatives daily for OIC?
Chronic use of stimulant laxatives should be avoided due to potential dependency. PAMORAs are preferred for long-term use.
Q5: Can OIC cause long-term bowel damage?
Yes, if unmanaged, it can lead to fecal impaction, hemorrhoids, anal fissures, and bowel obstruction.
Opioid-induced constipation is a pervasive and under-addressed side effect of opioid therapy. Understanding its unique pathophysiology, recognizing symptoms early, and implementing a stepwise treatment protocol are crucial to improving patient outcomes. Clinicians must tailor interventions to individual patient needs, prioritizing comfort and continuity of pain relief while minimizing gastrointestinal distress. Comprehensive management of OIC not only enhances quality of life but also ensures optimal adherence to pain management regimens.