Ophthalmia sympathetic, medically termed sympathetic ophthalmia, is a rare but serious bilateral granulomatous uveitis that occurs after penetrating trauma or intraocular surgery in one eye. The condition may lead to vision loss in both eyes if not identified and managed promptly. The unaffected eye, known as the sympathizing eye, becomes inflamed due to an autoimmune response triggered by exposure to ocular antigens from the injured eye, also called the exciting eye.

Etiology: Causes of Sympathetic Ophthalmia
The pathogenesis of ophthalmia sympathetic lies in immune system dysregulation following ocular trauma or surgery. It is believed that previously sequestered intraocular antigens—such as retinal S-antigen and interphotoreceptor retinoid-binding protein (IRBP)—are exposed to the immune system, leading to a delayed hypersensitivity reaction.
Common Triggers
- Penetrating ocular trauma
- Intraocular surgery (e.g., vitreoretinal or cataract surgery)
- Uveal prolapse
- Non-penetrating injuries (rarely)
Pathophysiology: Immune Mechanism Behind Sympathetic Ophthalmia
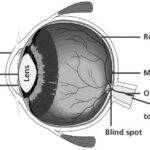
Once the integrity of the blood-ocular barrier is compromised, antigens from the uveal tract become accessible to antigen-presenting cells, leading to T-cell sensitization. This systemic immune response does not distinguish between the injured and uninjured eye, causing bilateral granulomatous inflammation of the uveal tract.
Clinical Features and Symptoms
Sympathetic ophthalmia usually develops 2 weeks to 2 months after trauma but can appear even years later. It presents with classic signs of chronic granulomatous uveitis, often affecting both anterior and posterior segments of the sympathizing eye.
Ocular Symptoms
- Blurred vision
- Photophobia
- Eye pain
- Redness
- Floaters
- Reduced visual acuity
Fundoscopic Findings
- Dalen-Fuchs nodules: Small yellow-white lesions at the level of the retinal pigment epithelium
- Serous retinal detachment
- Vitritis and choroiditis
Anterior Segment Signs
- Mutton-fat keratic precipitates
- Posterior synechiae
- Cells and flare in the anterior chamber
Diagnostic Criteria and Investigations
Early diagnosis of ophthalmia sympathetic is crucial to prevent bilateral blindness.
Clinical Diagnosis
Based on history of penetrating ocular trauma and bilateral granulomatous uveitis.
Diagnostic Tools
- OCT (Optical Coherence Tomography): Detects serous retinal detachments
- Fluorescein Angiography: Highlights retinal and choroidal inflammation
- Ultrasound B-scan: Useful in cases with opaque media
- MRI/CT: In complex or atypical cases
- Blood Tests: Rule out systemic autoimmune conditions (e.g., sarcoidosis, VKH syndrome)
Differential Diagnosis
Ophthalmia sympathetic must be differentiated from other causes of bilateral granulomatous uveitis:
- Vogt-Koyanagi-Harada (VKH) Syndrome
- Sarcoidosis
- Tuberculosis
- Syphilis
- Idiopathic uveitis
Management and Treatment Options
The primary goals in treatment are to preserve vision, control inflammation, and prevent recurrence.
Medical Management
Corticosteroids
- High-dose systemic steroids (e.g., oral prednisone or IV methylprednisolone)
- Topical steroids for anterior uveitis
Immunosuppressive Therapy
- Used when corticosteroids alone are insufficient
- Agents include azathioprine, methotrexate, cyclosporine, and mycophenolate mofetil
Biologic Agents
- TNF-alpha inhibitors (e.g., infliximab, adalimumab) in refractory cases
Surgical Intervention
Enucleation of the Injured Eye
- Preventive enucleation within 10–14 days post-injury may prevent onset
- Once inflammation in the sympathizing eye begins, enucleation is not beneficial
Prognosis and Long-Term Monitoring
With early diagnosis and aggressive treatment, visual outcomes can be favorable. However, delayed treatment often results in permanent visual impairment.
Factors Influencing Prognosis
- Timing of diagnosis
- Prompt initiation of immunosuppressive therapy
- Extent of ocular inflammation
- Patient adherence to follow-up and treatment
Long-term monitoring is essential due to the risk of relapse and complications such as:
- Cataract
- Glaucoma
- Retinal detachment
- Optic nerve damage
Preventive Measures
Although rare, the severity of sympathetic ophthalmia necessitates vigilance in all ocular trauma cases.
Preventive Strategies
- Immediate and appropriate management of eye injuries
- Judicious use of intraocular surgery
- Consideration of early enucleation in non-viable traumatized eyes
- Regular follow-up post-ocular trauma or surgery
Frequently Asked Questions
Q1: What is the earliest sign of ophthalmia sympathetic?
Blurred vision and photophobia in the uninjured eye following trauma are early warning signs.
Q2: How long after injury can sympathetic ophthalmia occur?
It typically appears within 2 months but may develop years later.
Q3: Is ophthalmia sympathetic curable?
While not curable, it can be controlled effectively with steroids and immunosuppressive therapy.
Q4: Can both eyes be lost to sympathetic ophthalmia?
Yes. If untreated, both eyes can suffer irreversible damage leading to bilateral blindness.
Q5: Is enucleation always necessary?
Not always. It’s considered when the injured eye is blind and painful or to prevent onset if inflammation hasn’t begun.
Ophthalmia sympathetic is a vision-threatening autoimmune condition triggered by ocular trauma or surgery. Timely recognition, aggressive immunosuppression, and preventive strategies are paramount in preserving visual function. Clinicians must maintain a high index of suspicion in post-trauma cases and institute prompt, targeted therapy to mitigate this rare yet devastating disease.