Open-angle glaucoma, also known as primary open-angle glaucoma (POAG), is a chronic, progressive optic neuropathy characterized by increased intraocular pressure (IOP) and subsequent damage to the optic nerve. It is the most prevalent form of glaucoma, accounting for approximately 90% of all glaucoma cases worldwide.
Despite its prevalence, POAG is often termed the “silent thief of sight” due to its asymptomatic progression until advanced stages. Without timely intervention, it can lead to irreversible vision loss. Understanding the condition’s pathophysiology, risk factors, and management is crucial for early detection and treatment.
Pathophysiology of Open-Angle Glaucoma
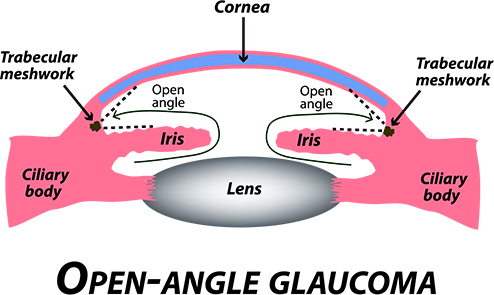
In POAG, the trabecular meshwork—the primary drainage route for aqueous humor—becomes less efficient, leading to elevated intraocular pressure. This pressure damages the retinal ganglion cell axons at the optic nerve head.
This damage leads to progressive loss of the visual field, typically starting in the peripheral vision, while central vision remains unaffected until the late stages.
Risk Factors for Primary Open-Angle Glaucoma
A number of modifiable and non-modifiable factors contribute to the development of POAG:
Non-Modifiable Risk Factors:
- Age over 40
- Family history of glaucoma
- African, Hispanic, or Asian descent
- Thin central corneal thickness
- Myopia (nearsightedness)
Modifiable Risk Factors:
- Elevated IOP
- Systemic hypertension
- Diabetes mellitus
- Prolonged corticosteroid use
- Obstructive sleep apnea
Early identification of high-risk individuals enables timely screening and intervention.
Clinical Presentation and Symptoms
Open-angle glaucoma progresses gradually, and symptoms often go unnoticed until substantial vision loss has occurred.
Early Stage:
- Asymptomatic
- Normal central vision
Intermediate Stage:
- Subtle loss of peripheral vision
- May be discovered during routine eye exams
Advanced Stage:
- Tunnel vision
- Central vision eventually compromised
- Difficulty in low-light conditions
Diagnostic Evaluation of Open-Angle Glaucoma
A definitive diagnosis of POAG relies on a comprehensive ophthalmic examination, incorporating structural and functional tests:
1. Tonometry
- Measures intraocular pressure (IOP)
- Normal IOP: 10–21 mmHg
- POAG may occur with normal IOP (normal-tension glaucoma)
2. Ophthalmoscopy
- Visualizes optic nerve head for cupping and pallor
3. Optical Coherence Tomography (OCT)
- Provides cross-sectional imaging of the retinal nerve fiber layer (RNFL)
- Detects early structural changes
4. Visual Field Testing (Perimetry)
- Detects functional loss in peripheral vision
- Humphrey Field Analyzer is most commonly used
5. Gonioscopy
- Confirms that the angle between iris and cornea is open
- Distinguishes POAG from angle-closure glaucoma
Stages of Open-Angle Glaucoma
| Stage | Description | Visual Field Impact |
|---|---|---|
| Early | Optic nerve damage with no symptoms | None or subtle |
| Moderate | Noticeable optic nerve cupping and RNFL thinning | Peripheral field loss |
| Advanced | Severe optic nerve damage | Tunnel vision |
| End-stage | Total optic atrophy | Complete vision loss |
Treatment Options for Open-Angle Glaucoma
The goal of treatment is to reduce intraocular pressure, thereby preventing further optic nerve damage.
1. Medications
Primarily in the form of eye drops, these drugs either reduce aqueous humor production or increase outflow.
| Drug Class | Mechanism | Example |
|---|---|---|
| Prostaglandin analogs | ↑ Uveoscleral outflow | Latanoprost, Travoprost |
| Beta-blockers | ↓ Aqueous production | Timolol |
| Alpha-agonists | ↓ Production & ↑ outflow | Brimonidine |
| Carbonic anhydrase inhibitors | ↓ Production | Dorzolamide, Brinzolamide |
| Rho kinase inhibitors | ↑ Trabecular outflow | Netarsudil |
2. Laser Therapy
- Selective Laser Trabeculoplasty (SLT): Increases trabecular outflow
- Often used when medications are insufficient or not tolerated
3. Surgical Management
- Trabeculectomy: Creates a new drainage path for aqueous humor
- Glaucoma drainage devices: Implants used when trabeculectomy fails
- Minimally Invasive Glaucoma Surgery (MIGS): Safer with faster recovery
Monitoring and Prognosis
Regular follow-up is essential for monitoring disease progression. This includes:
- Quarterly to biannual visual field testing
- OCT imaging every 6–12 months
- IOP monitoring at each visit
Prognosis:
- With early detection and consistent treatment, vision loss can be minimized
- However, any existing vision loss is irreversible
Prevention and Patient Education
While open-angle glaucoma cannot be prevented entirely, regular eye examinations and risk factor modification significantly reduce the burden of disease.
Key Preventive Measures:
- Routine screening for those over 40
- Control of systemic diseases like diabetes and hypertension
- Avoid long-term use of corticosteroids unless medically necessary
- Educate patients about compliance with therapy
Frequently Asked Questions:
Q1: Can open-angle glaucoma be cured?
No, it cannot be cured, but progression can be effectively controlled with medication, laser, or surgery.
Q2: Is open-angle glaucoma hereditary?
Yes, family history significantly increases risk. First-degree relatives should undergo regular screening.
Q3: Can you have glaucoma with normal eye pressure?
Yes, normal-tension glaucoma is a variant of POAG where optic nerve damage occurs at normal IOP levels.
Q4: Are both eyes affected simultaneously?
POAG typically affects both eyes, though not always symmetrically.
Q5: What happens if glaucoma is left untreated?
Untreated glaucoma leads to progressive and irreversible vision loss, ultimately resulting in blindness.
Open-angle glaucoma is a leading cause of irreversible blindness worldwide. Its silent onset and progressive nature necessitate regular ophthalmic evaluation, especially in high-risk groups. Through early detection, individualized therapy, and consistent monitoring, we can preserve vision and significantly enhance the quality of life for affected individuals.