Oligoarticular juvenile idiopathic arthritis (JIA) is the most common subtype of juvenile idiopathic arthritis, a chronic autoimmune disorder affecting children under the age of 16. Defined by the involvement of four or fewer joints within the first six months of disease onset, oligoarticular JIA is further classified into persistent and extended forms based on disease progression. It primarily affects large joints, especially the knees and ankles, and has a notable female predominance.
This condition may present with subtle clinical signs, and early recognition is critical for preventing joint damage and minimizing systemic complications.
Classification: Persistent vs. Extended Oligoarticular JIA
- Persistent Oligoarticular JIA: Joint involvement remains limited to four or fewer joints during the entire course.
- Extended Oligoarticular JIA: More than four joints become affected after the initial six months, often leading to more severe outcomes.
Etiology and Risk Factors
While the exact cause of oligoarticular JIA remains unknown, the disorder is believed to result from a combination of genetic susceptibility and immune dysregulation, often triggered by environmental factors.
Genetic and Environmental Influences
- HLA associations: Specific HLA class II alleles (e.g., HLA-DRB1*11) are linked with increased susceptibility.
- Autoantibody presence: Antinuclear antibodies (ANA) are frequently detected, especially in females, indicating higher risk of uveitis.
- Infections and environmental triggers: While not definitive, infections may initiate or exacerbate immune responses in genetically predisposed individuals.
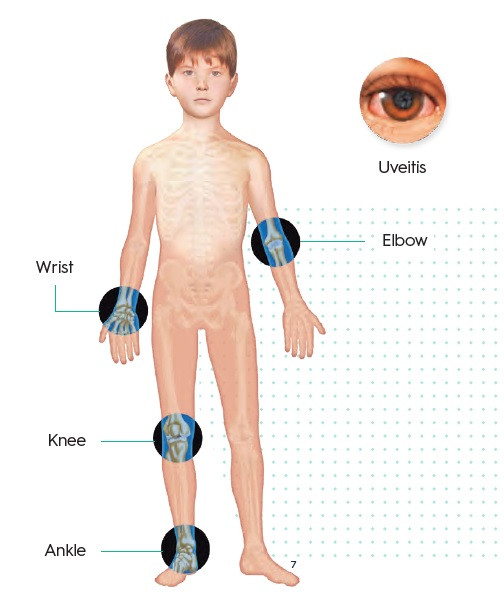
Clinical Features and Symptoms
Oligoarticular JIA typically presents in toddlers and young children, often between the ages of 2 and 4 years. Symptoms may be subtle and easily overlooked without vigilant examination.
Key Symptoms:
- Asymmetric joint involvement, especially the knee, ankle, or wrist
- Morning stiffness or difficulty moving after rest
- Joint swelling and limited motion
- Minimal or absent pain, often leading to underreporting
- Limping or avoidance of using a limb
- No systemic symptoms like fever or rash (unlike systemic JIA)
Ocular Complications: Risk of Uveitis
Children with oligoarticular JIA are at high risk of chronic anterior uveitis, an eye inflammation that can lead to vision loss if untreated. The risk is especially elevated in:
- ANA-positive patients
- Females
- Children under 7 years at disease onset
Routine ophthalmologic screening is essential, even in asymptomatic cases, due to the often silent progression of ocular involvement.
Diagnostic Approach
Early diagnosis relies on a combination of clinical evaluation, laboratory testing, and imaging, as there is no single confirmatory test.
Clinical Criteria:
- Age of onset <16 years
- Arthritis in ≤4 joints for the first six months
- Duration ≥6 weeks
Laboratory Tests:
| Test | Purpose |
|---|---|
| ANA | Indicates higher risk of uveitis |
| ESR/CRP | Markers of systemic inflammation |
| Rheumatoid factor (RF) | Typically negative in oligoarticular JIA |
| HLA typing | May support diagnosis in some cases |
Imaging Studies:
- Ultrasound: Detects joint effusion and synovitis
- MRI: Provides detailed evaluation of early joint changes, especially in the hip or jaw
Treatment and Management Strategies
Management of oligoarticular JIA aims to control inflammation, preserve joint function, and prevent complications. Treatment is guided by disease severity and progression.
First-Line Treatment:
1. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
- Reduce pain and inflammation
- Examples: Naproxen, ibuprofen
2. Intra-Articular Corticosteroid Injections
- Rapid relief with minimal systemic side effects
- Effective for isolated joint involvement
Second-Line and Long-Term Therapy:
3. Disease-Modifying Antirheumatic Drugs (DMARDs)
- Methotrexate is the most commonly used DMARD for extended or refractory cases.
4. Biologic Agents
- Indicated in patients who do not respond to methotrexate.
- Includes TNF inhibitors like etanercept or adalimumab.
Adjunctive Care:
- Physical therapy: Prevents joint stiffness and maintains function
- Ophthalmology monitoring: Every 3–12 months based on uveitis risk
Prognosis and Long-Term Outlook
Most children with persistent oligoarticular JIA experience a favorable outcome with minimal joint damage when treated early. However, those with extended oligoarticular JIA or uveitis complications may face more complex disease courses.
Prognostic Indicators:
| Favorable Factors | Poor Prognostic Markers |
|---|---|
| Limited joint involvement | Extended joint involvement |
| Early treatment | ANA positivity with uveitis |
| Good therapeutic response | Delay in diagnosis |
Regular follow-up is essential for early detection of flare-ups, eye complications, or medication side effects.
Lifestyle Considerations and Parental Guidance
- Activity modification is necessary during active flares, but regular exercise is encouraged to maintain mobility.
- Nutritional support with vitamin D and calcium helps in bone health.
- Parents should maintain detailed records of symptoms, medications, and specialist appointments to aid in comprehensive care.
Frequently Asked Questions
Q1: Can oligoarticular JIA go away on its own?
Some cases enter remission, especially with early intervention, but long-term monitoring is necessary.
Q2: How often should children with JIA have eye exams?
Typically every 3 to 12 months depending on ANA status and age, as guided by a pediatric ophthalmologist.
Q3: Is oligoarticular JIA the same as rheumatoid arthritis?
No. While both are autoimmune arthritides, they differ in onset, symptoms, and systemic involvement.
Q4: Can children with JIA participate in sports?
Yes, with guidance from physicians and physical therapists to prevent joint strain.
Q5: What is the difference between oligoarticular and polyarticular JIA?
Oligoarticular JIA affects ≤4 joints initially; polyarticular JIA involves ≥5 joints from the onset.
Oligoarticular juvenile idiopathic arthritis represents a significant pediatric autoimmune disorder with distinct clinical and prognostic features. Prompt diagnosis, routine screening for ocular involvement, and a personalized treatment approach are crucial to ensure optimal outcomes. By fostering awareness and maintaining comprehensive care, we can improve quality of life and functional independence for children living with this condition.