Allergic rhinitis, commonly known as hay fever, is a hypersensitivity reaction of the nasal mucosa to allergens such as pollen, dust mites, pet dander, or mold spores. Beyond nasal symptoms, a significant subset of patients experience ocular symptoms associated with allergic rhinitis, which can substantially impair quality of life. These symptoms often involve inflammation of the conjunctiva and periorbital tissues, collectively contributing to what is termed allergic conjunctivitis.
Prevalence and Impact of Ocular Symptoms in Allergic Rhinitis
Ocular symptoms are present in approximately 60–70% of allergic rhinitis cases. These manifestations, especially during peak pollen seasons, lead to discomfort, visual disturbances, and reduced productivity. The prevalence is notably higher in seasonal allergic rhinitis (SAR) compared to perennial allergic rhinitis (PAR) due to periodic exposure to aeroallergens.
Pathophysiology of Ocular Allergic Responses
Allergic ocular symptoms result from a Type I hypersensitivity reaction mediated by IgE antibodies. Upon exposure to allergens, mast cells degranulate and release histamine, prostaglandins, and leukotrienes, which lead to vasodilation, increased vascular permeability, and sensory nerve stimulation.
Phases of the Allergic Response:
- Sensitization Phase
- Allergen exposure triggers IgE production, which binds to mast cells.
- Early Phase Reaction (within minutes)
- Histamine release causes itchy eyes, redness, and tearing.
- Late Phase Reaction (4–24 hours)
- Recruitment of eosinophils and cytokines exacerbates inflammation and swelling.
Common Ocular Symptoms Associated with Allergic Rhinitis
1. Itchy Eyes (Ocular Pruritus)
Often the earliest and most persistent symptom; bilateral itching worsens with rubbing.
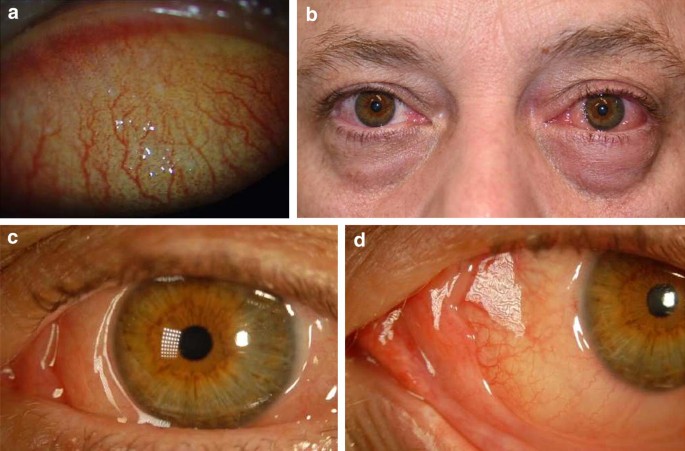
2. Redness (Hyperemia)
Dilation of conjunctival vessels leads to visible eye redness.
3. Watery Eyes (Epiphora)
Excessive tearing caused by irritation and inflammation of the lacrimal glands.
4. Swelling (Chemosis and Periorbital Edema)
Conjunctival edema may cause ballooning of the eye surface and puffiness around the eyes.
5. Burning Sensation and Grittiness
Inflammation and dryness cause discomfort and a foreign body sensation.
6. Light Sensitivity (Photophobia)
Occurs in more severe or chronic allergic responses.
Differentiating Ocular Allergy from Other Eye Conditions
Differential diagnosis is crucial to avoid mismanagement. Ocular symptoms of allergic rhinitis must be distinguished from:
| Condition | Key Features |
|---|---|
| Infectious Conjunctivitis | Purulent discharge, unilateral onset, no itching |
| Dry Eye Syndrome | Foreign body sensation, minimal redness, worsens with screen time |
| Blepharitis | Eyelid crusting, meibomian gland dysfunction |
| Vernal Keratoconjunctivitis | Chronic, typically in young males, with giant papillae |
Diagnosis of Allergic Eye Symptoms
Clinical Evaluation:
- Detailed allergy history (onset, triggers, seasonality)
- Assessment of nasal and ocular symptoms
- Visual inspection under slit-lamp microscopy reveals:
- Papillary hypertrophy
- Conjunctival hyperemia
- Chemosis
Allergy Testing:
- Skin Prick Tests or Specific IgE Blood Tests to identify sensitizing allergens
- Tear eosinophil count may support allergic diagnosis
Medical Management of Ocular Symptoms
1. Topical Antihistamines
- Olopatadine, Ketotifen, and Azelastine
- Provide rapid relief from itching and redness
2. Mast Cell Stabilizers
- Nedocromil or Cromolyn sodium
- Prevent mast cell degranulation; useful for long-term control
3. Dual-Action Agents
- Combine antihistaminic and mast cell stabilizing effects
- Examples: Epinastine, Bepotastine
4. Artificial Tears
- Dilute allergens and soothe irritated ocular surface
5. Intranasal Corticosteroids
- Reduce both nasal and ocular inflammation
- Fluticasone or Mometasone often effective
6. Oral Antihistamines
- Second-generation agents (Loratadine, Fexofenadine) preferred for minimal drowsiness
7. Immunotherapy
- Allergen-specific immunotherapy (subcutaneous or sublingual)
- Offers long-term control in sensitized individuals
Lifestyle Modifications and Allergen Avoidance
Reducing allergen exposure is foundational in managing ocular symptoms:
- Close windows during high pollen counts
- Use HEPA filters in air conditioning units
- Wash hands and face after outdoor activities
- Avoid rubbing the eyes to prevent worsening symptoms
- Cold compresses can provide temporary relief from swelling and itching
Pediatric Considerations
In children, allergic rhinitis and ocular symptoms may present with:
- Eye rubbing and blinking
- Behavioral changes due to discomfort
- Associated atopic conditions (eczema, asthma)
Pediatric patients require weight-adjusted dosing and careful monitoring for side effects from topical or systemic therapies.
Complications and Long-Term Consequences
Though typically benign, chronic or untreated ocular allergic symptoms can lead to:
- Keratitis
- Corneal epithelial damage
- Vision disturbances
- Secondary infections from excessive eye rubbing
Timely intervention prevents ocular surface damage and preserves visual function.
Frequently Asked Questions
Q1: Can allergic rhinitis cause eye pain?
While true pain is uncommon, severe itching and burning may mimic discomfort. Pain suggests a need to rule out infection or other ocular pathology.
Q2: Are eye drops safe for daily use in allergic rhinitis?
Yes, preservative-free formulations and dual-action agents are generally safe for long-term use under medical supervision.
Q3: Do all patients with allergic rhinitis experience ocular symptoms?
No, but a significant portion—especially those with seasonal triggers—do report eye-related complaints.
Q4: Can allergic rhinitis affect vision?
Temporary blurring may occur due to tearing or swelling, but permanent vision loss is rare unless complications develop.
Q5: Are there natural remedies for allergic eye symptoms?
Cold compresses, saline rinses, and avoiding known allergens can help. However, medical therapy remains the mainstay.
Ocular symptoms associated with allergic rhinitis are a common yet often underestimated component of allergic disease. Accurate diagnosis and a multidisciplinary management plan—including pharmacotherapy, allergen avoidance, and long-term control strategies—are essential to alleviate discomfort and enhance patient quality of life. Integrating both ophthalmological and immunological insights ensures a comprehensive approach to this prevalent condition.