Ocular irritation refers to a condition characterized by discomfort, stinging, itching, or burning sensations in the eyes. Often a symptom of underlying pathology, it may result from environmental triggers, systemic conditions, or localized eye disorders. Recognizing the etiology and implementing prompt management are vital to avoid complications and restore ocular comfort.
Common Causes of Ocular Irritation
Several internal and external factors can contribute to eye irritation. Identifying the root cause is crucial for effective relief and prevention of recurrence.
Environmental and Occupational Factors
- Air pollution and allergens (dust, pollen, smoke)
- Exposure to chemicals or fumes in industrial settings
- Prolonged screen time leading to digital eye strain
- Dry indoor environments due to air conditioning or heating
Ocular Surface Disorders
- Dry Eye Syndrome (Keratoconjunctivitis Sicca): Caused by insufficient tear production or rapid evaporation.
- Blepharitis: Inflammation of the eyelid margins, often due to bacterial colonization or meibomian gland dysfunction.
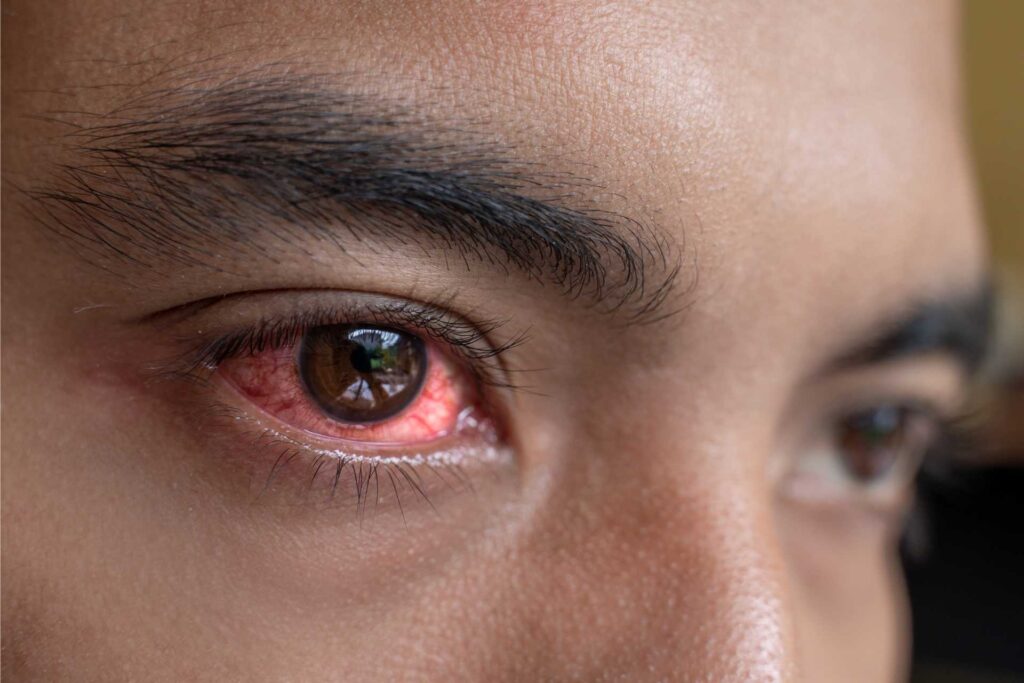
- Conjunctivitis: Viral, bacterial, or allergic inflammation of the conjunctiva causing redness and discomfort.
- Corneal Abrasions: Minor injuries leading to pain, photophobia, and foreign body sensation.
Contact Lens-Related Irritation
- Poor hygiene, overuse, or ill-fitting contact lenses may induce corneal hypoxia, infection, or mechanical irritation.
Systemic and Allergic Conditions
- Autoimmune diseases like Sjögren’s syndrome or lupus
- Allergic rhinitis and atopic conditions leading to ocular hypersensitivity
- Medication-induced irritation, especially from topical glaucoma drops or preservatives like benzalkonium chloride
Symptoms of Ocular Irritation
Patients typically present with a variety of overlapping symptoms that vary in intensity and duration:
- Persistent itching or burning sensation
- Redness (hyperemia) of the conjunctiva
- Excessive tearing or watery eyes
- Dryness or foreign body sensation
- Photophobia (light sensitivity)
- Blurred vision during episodes of irritation
- Mucous discharge, especially in allergic conjunctivitis
- Involuntary blinking or eye rubbing
Diagnostic Evaluation of Eye Irritation
Proper diagnosis involves a thorough clinical history and specialized ophthalmic examinations.
Clinical Examination Tools
- Slit-lamp Biomicroscopy: Evaluates the ocular surface, tear film, conjunctiva, and cornea.
- Fluorescein staining: Detects corneal epithelial defects and dry spots.
- Schirmer’s test: Measures tear production for dry eye diagnosis.
- Tear Break-Up Time (TBUT): Assesses tear film stability.
- Conjunctival swab or scraping: Identifies microbial or allergic etiology.
Effective Treatment Strategies for Ocular Irritation
Treatment must be directed toward the underlying cause to achieve lasting relief.
Artificial Tears and Lubricants
- Preservative-free formulations recommended for chronic use
- Gel or ointment-based drops for nighttime protection
- Lipid-enhanced drops to improve tear film stability
Anti-Inflammatory Therapy
- Topical corticosteroids for short-term use in moderate-to-severe cases
- Cyclosporine A (Restasis) and lifitegrast for chronic dry eye linked to inflammation
- Antihistamine eye drops (olopatadine, ketotifen) for allergic causes
Managing Blepharitis and Meibomian Gland Dysfunction
- Lid hygiene with warm compresses and eyelid scrubs
- Oral tetracyclines (e.g., doxycycline) for meibomian gland inflammation
- In-office treatments: LipiFlow, IPL therapy
Contact Lens Optimization
- Switch to daily disposable lenses
- Use preservative-free contact lens solutions
- Ensure proper fitting and reduced wearing time
Treating Underlying Systemic Conditions
- Coordinate with rheumatologists or allergists for autoimmune or allergic conditions
- Adjust systemic medications contributing to ocular dryness
Preventive Measures for Ocular Irritation
Implementing preventive strategies is essential to minimize recurrence and maintain ocular comfort.
Environmental Adjustments
- Use humidifiers in dry indoor environments
- Avoid direct exposure to air vents or fans
- Wear protective eyewear in dusty or windy conditions
- Reduce screen time and practice the 20-20-20 rule
Personal Hygiene and Eye Care
- Avoid touching or rubbing eyes
- Regularly clean makeup tools and replace eye cosmetics
- Follow strict contact lens hygiene protocols
- Wash hands frequently to prevent infectious conjunctivitis
Nutritional and Lifestyle Support
- Omega-3 fatty acids (flaxseed oil, fish oil) support tear production
- Stay hydrated to enhance mucous membrane function
- Use blue-light blocking glasses to reduce digital eye strain
Complications Arising from Persistent Ocular Irritation
Neglected or mismanaged ocular irritation can lead to:
- Corneal ulcers or erosions
- Recurrent eye infections
- Scarring of ocular tissues
- Reduced visual acuity
- Increased risk of chronic dry eye syndrome
Timely management prevents progression to more severe ocular pathology.
Frequently Asked Questions:
Q1: What is the most common cause of ocular irritation?
Dry eye syndrome and environmental exposure are among the leading causes.
Q2: Can ocular irritation be a sign of something serious?
Yes, chronic irritation may indicate autoimmune diseases or infections requiring medical attention.
Q3: Are over-the-counter eye drops safe for regular use?
Preservative-free artificial tears are generally safe, but medicated drops should be used under medical supervision.
Q4: How long does ocular irritation typically last?
Mild cases resolve in hours to days, while chronic conditions may require long-term management.
Q5: When should I consult an ophthalmologist for irritated eyes?
Seek professional evaluation if symptoms persist beyond a few days or worsen despite initial treatment.
Ocular irritation, though often considered a minor inconvenience, may signal deeper ocular or systemic issues. A comprehensive understanding of its multifactorial origins—ranging from dry eyes and allergens to autoimmune disorders—guides us in delivering targeted treatment. With timely intervention, preventive care, and patient education, we can ensure long-term ocular comfort and preserve vision.

