Ocular inflammation refers to the immune-mediated or infectious inflammation of any part of the eye. It encompasses a broad spectrum of conditions, ranging from mild surface irritation to sight-threatening intraocular inflammation. Prompt diagnosis and management are crucial to prevent long-term visual impairment.

Types of Ocular Inflammation
Ocular inflammation can affect various anatomical structures. Based on the site of involvement, it is categorized as follows:
1. Anterior Segment Inflammation
- Conjunctivitis: Inflammation of the conjunctiva, typically viral or bacterial.
- Keratitis: Corneal inflammation, often infectious (herpes simplex, bacterial, fungal).
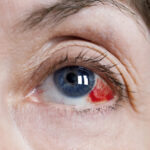
- Episcleritis and Scleritis: Superficial or deep inflammation of the scleral tissues.
- Iritis/Anterior Uveitis: Inflammation of the iris, often autoimmune in nature.
2. Intermediate Inflammation
- Intermediate Uveitis: Inflammation centered around the vitreous and peripheral retina.
Associated with multiple sclerosis, sarcoidosis, or idiopathic causes.
3. Posterior Segment Inflammation
- Choroiditis: Inflammation of the choroid layer.
- Retinitis: Involvement of the retina due to infections (toxoplasmosis, CMV).
- Posterior Uveitis: Includes both choroiditis and retinitis.
4. Panuveitis
- Involves all layers of the uveal tract (iris, ciliary body, and choroid).
Often associated with systemic autoimmune conditions or infections.
Common Causes and Risk Factors
Ocular inflammation can result from infectious, autoimmune, or idiopathic origins. Recognizing the underlying etiology is essential for appropriate treatment.
Infectious Causes
- Bacterial: Staphylococcus aureus, Mycobacterium tuberculosis
- Viral: Herpes simplex virus, Varicella-zoster virus, CMV
- Fungal: Candida, Aspergillus
- Parasitic: Toxoplasma gondii
Autoimmune and Systemic Associations
- Rheumatoid arthritis
- Ankylosing spondylitis
- Behçet’s disease
- Sarcoidosis
- Systemic lupus erythematosus
- Inflammatory bowel disease
Environmental and Other Factors
- Trauma or ocular surgery
- Contact lens misuse
- Drug-induced reactions
- Idiopathic (no identifiable cause)
Symptoms and Clinical Features
The symptoms vary depending on the location and severity of the inflammation.
| Location | Key Symptoms |
|---|---|
| Anterior Uveitis | Eye pain, photophobia, redness, blurred vision |
| Intermediate Uveitis | Floaters, mild vision loss |
| Posterior Uveitis | Blurred vision, floaters, scotomas |
| Panuveitis | Severe vision loss, pain, photophobia |
| Scleritis | Deep eye pain, tenderness, red eye |
| Keratitis | Pain, tearing, corneal opacity |
Diagnostic Evaluation of Ocular Inflammation
Early and precise diagnosis is critical to preserving visual function.
Clinical Examination
- Slit-lamp biomicroscopy: Evaluates anterior chamber cells, flare, and keratic precipitates.
- Fundus examination: Detects vitreous haze, choroidal lesions, and retinal vasculitis.
- Tonometry: Measures intraocular pressure, which may be elevated or decreased.
Imaging and Ancillary Tests
- Optical Coherence Tomography (OCT): Assesses retinal and choroidal thickness.
- Fundus Fluorescein Angiography (FFA): Visualizes retinal vascular leakage.
- Ultrasound B-scan: Useful in media opacity.
- Anterior chamber or vitreous tap: For microbiological diagnosis in infectious cases.
Systemic Work-Up
- Complete blood count (CBC)
- ESR, CRP
- HLA typing (e.g., HLA-B27)
- Chest X-ray or CT (for TB, sarcoidosis)
- Serologic tests (ANA, RF, VDRL, HIV, toxoplasma IgG/IgM)
Advanced Treatment Approaches
Treatment depends on the type, severity, and underlying cause of inflammation.
Corticosteroids
- Topical: First-line for anterior segment inflammation (prednisolone acetate)
- Periocular or intravitreal injection: For intermediate/posterior involvement
- Systemic (oral or IV methylprednisolone): In severe or refractory cases
Immunosuppressive Agents
Used for chronic or steroid-resistant inflammation, particularly in autoimmune uveitis.
- Methotrexate
- Azathioprine
- Mycophenolate mofetil
- Cyclosporine
Biologic Therapies
Reserved for severe, refractory, or sight-threatening uveitis.
- Anti-TNF agents (e.g., infliximab, adalimumab)
- Interleukin inhibitors (e.g., tocilizumab)
Antimicrobial Therapy
Initiated in proven or suspected infectious cases:
- Antibiotics: Tuberculosis (Rifampicin, Isoniazid, etc.), syphilis (penicillin)
- Antivirals: Herpetic infections (acyclovir, ganciclovir)
- Antifungals: Amphotericin B, voriconazole
- Antiparasitics: Pyrimethamine, sulfadiazine for toxoplasmosis
Complications of Untreated Ocular Inflammation
Delayed or inadequate management may result in irreversible damage:
- Cataract formation
- Secondary glaucoma
- Cystoid macular edema
- Retinal detachment
- Optic nerve atrophy
- Permanent vision loss
Monitoring and Follow-Up
Management does not end with resolution of acute symptoms. Continuous follow-up is mandatory to:
- Monitor for recurrence or chronicity
- Adjust immunosuppressive therapy
- Detect and manage complications early
- Evaluate systemic disease progression
Recommended follow-up interval:
- Active inflammation: Weekly or biweekly
- Stable/chronic cases: Every 1–3 months
- After tapering steroids: Monthly until stable
Prevention and Patient Education
- Avoid self-medication with steroids
- Comply with follow-up visits and prescribed therapies
- Use protective eyewear in high-risk occupations
- Practice good hygiene with contact lenses
- Report any new ocular symptoms promptly
Frequently Asked Questions
Q1: Can ocular inflammation go away on its own?
Mild cases like episcleritis may resolve spontaneously, but most require treatment to prevent progression.
Q2: Is ocular inflammation contagious?
Only infectious forms like viral conjunctivitis are contagious. Autoimmune types are not.
Q3: Does uveitis mean I have an autoimmune disease?
Not always. However, uveitis often serves as an early sign of systemic autoimmune conditions.
Q4: Can ocular inflammation recur?
Yes. Chronic and recurrent inflammation is common, particularly in autoimmune-related cases.
Q5: Is it safe to use steroid eye drops long-term?
Long-term use requires close supervision due to risks like cataract and glaucoma.
Ocular inflammation is a potentially vision-threatening condition that demands timely, multidisciplinary care. By integrating advanced diagnostics, tailored therapy, and vigilant monitoring, we can significantly improve patient outcomes. A holistic approach addressing both ocular and systemic health is imperative to ensure long-term visual preservation and quality of life.