Ocular hypertension refers to a condition in which the intraocular pressure (IOP) within the eye is consistently higher than the normal range, typically above 21 mmHg, without any detectable damage to the optic nerve or visual field loss. Though not a disease in itself, ocular hypertension is a critical risk factor for primary open-angle glaucoma, the leading cause of irreversible blindness worldwide.
Persistent elevated IOP requires ongoing evaluation and management to prevent progression to glaucomatous optic neuropathy.
Understanding Intraocular Pressure (IOP)
Intraocular pressure is the fluid pressure inside the eye, maintained by the balance between the production and drainage of aqueous humor, a clear fluid produced by the ciliary body.
Normal vs Elevated IOP:
- Normal IOP: 10 to 21 mmHg
- Ocular Hypertension: Above 21 mmHg with normal optic nerve and visual fields
- Glaucoma: Elevated IOP with optic nerve damage or visual field loss
Disruption in this pathway, especially at the trabecular meshwork, leads to increased resistance and subsequently raised eye pressure.
Causes and Risk Factors of Ocular Hypertension
Primary Causes
- Reduced outflow of aqueous humor
- Overproduction of aqueous humor
- Age-related changes in drainage structures
- Steroid-induced ocular hypertension
Risk Factors
- Age > 40 years
- African or Hispanic ancestry
- Family history of glaucoma
- Thin central corneal thickness (<555 microns)
- Diabetes, hypertension, or high myopia
- Prolonged corticosteroid use (topical or systemic)
- Trauma or eye surgery history
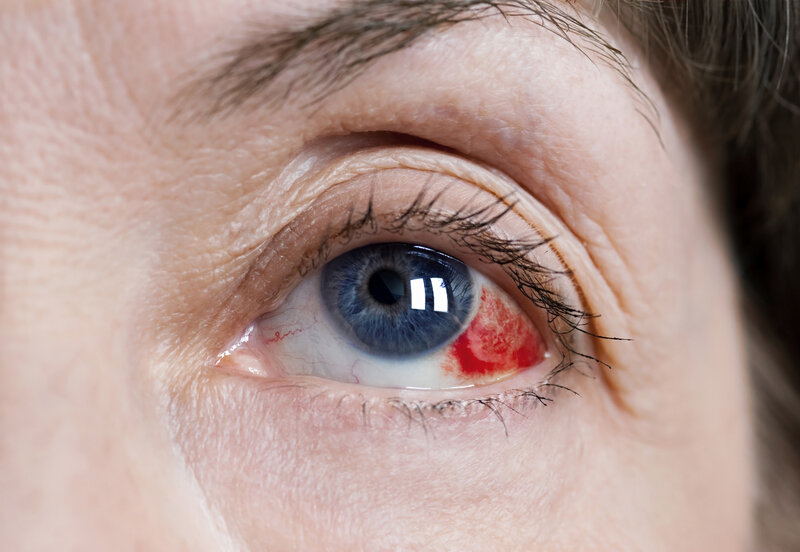
Symptoms and Clinical Presentation
Ocular hypertension typically presents without symptoms, making it a silent condition. Unlike acute angle-closure glaucoma, there is no pain, redness, or blurred vision in most cases. It is often diagnosed during routine comprehensive eye examinations using tonometry and optic nerve assessments.
Diagnostic Approach to Ocular Hypertension
Comprehensive Eye Exam Includes:
- Tonometry: Measures IOP via applanation or rebound techniques
- Pachymetry: Measures central corneal thickness, as thinner corneas can underestimate true IOP
- Gonioscopy: Examines anterior chamber angle to rule out angle-closure mechanisms
- Ophthalmoscopy: Assesses optic disc for cupping or nerve fiber layer changes
- Visual Field Testing: Detects early functional loss not visible on imaging
- Optical Coherence Tomography (OCT): Measures retinal nerve fiber layer and optic nerve head
Diagnostic Criteria for Ocular Hypertension:
- IOP consistently above 21 mmHg
- Normal optic disc appearance
- No visual field defects
- Open anterior chamber angle
- Absence of secondary causes
Ocular Hypertension vs Glaucoma
| Feature | Ocular Hypertension | Glaucoma |
|---|---|---|
| IOP | Elevated | Elevated or normal |
| Optic Nerve | Normal | Damaged |
| Visual Field | Normal | Abnormal |
| Symptoms | None | Often asymptomatic; late-stage vision loss |
| Risk of Progression | Present | Active disease |
Management of Ocular Hypertension
Observation vs Treatment
Not all cases of ocular hypertension require treatment. The decision is based on individual risk factors for progression to glaucoma.
Indications for Treatment
- IOP > 25 mmHg
- Thin central cornea
- Positive family history of glaucoma
- Suspicious optic disc
- High-risk racial background
- Comorbid systemic diseases
Treatment Options
1. Topical Medications
- Prostaglandin Analogues (e.g., latanoprost): First-line for lowering IOP
- Beta-blockers (e.g., timolol): Reduce aqueous production
- Alpha-agonists (e.g., brimonidine): Reduce production and increase outflow
- Carbonic Anhydrase Inhibitors (e.g., dorzolamide): Decrease fluid production
- Rho Kinase Inhibitors: New class targeting trabecular meshwork resistance
2. Laser Therapy
- Selective Laser Trabeculoplasty (SLT): Enhances outflow via trabecular meshwork
- Safe and repeatable; can be used as primary or adjunctive therapy
3. Surgical Intervention
Reserved for cases where medications and laser therapy fail.
- Trabeculectomy
- Minimally Invasive Glaucoma Surgery (MIGS)
Monitoring and Long-Term Follow-Up
Patients with ocular hypertension require lifelong monitoring, even if no treatment is initiated. Frequency depends on individual risk:
- Low-risk: Every 6–12 months
- Moderate to high-risk: Every 3–6 months
- Post-treatment follow-up: Within 4–6 weeks to assess response
Monitoring includes:
- Regular IOP checks
- Optic nerve imaging
- Visual field analysis
- Corneal thickness assessment (annually or as needed)
Lifestyle and Preventive Strategies
While lifestyle alone cannot reduce IOP significantly, it complements medical management:
- Exercise: Regular aerobic activity may reduce IOP
- Avoid smoking and reduce caffeine intake
- Protect eyes from trauma
- Manage systemic health (hypertension, diabetes)
- Adherence to follow-up schedules and medications
Frequently Asked Questions
Q1: Can ocular hypertension turn into glaucoma?
Yes, especially if left untreated. Around 10% of patients with ocular hypertension develop glaucoma within 5 years.
Q2: Is ocular hypertension reversible?
While IOP can be controlled, the condition requires continuous monitoring to prevent irreversible damage.
Q3: Are eye drops for ocular hypertension safe long-term?
Most are safe with proper use, but some may cause redness, irritation, or systemic side effects, which should be discussed with an ophthalmologist.
Q4: How do I know if I have high eye pressure?
Only through an eye exam with tonometry; the condition does not present symptoms.
Q5: Can ocular hypertension affect both eyes?
Yes, it commonly affects both eyes symmetrically, though variations can occur.
Ocular hypertension serves as a critical precursor to glaucoma, making early diagnosis and appropriate management vital in preserving long-term vision. With timely intervention, risk stratification, and regular surveillance, we can effectively control intraocular pressure and prevent the devastating consequences of optic nerve damage. Comprehensive patient education and adherence to treatment regimens remain pivotal in ensuring successful outcomes.