Obstructive Sleep Apnea Syndrome (OSA) is a serious sleep-related breathing disorder characterized by repetitive episodes of upper airway obstruction during sleep. These episodes, often associated with a reduction (hypopnea) or complete cessation (apnea) of airflow, lead to fragmented sleep, intermittent hypoxemia, and excessive daytime sleepiness. OSA poses significant health risks, including cardiovascular disease, cognitive impairment, and metabolic dysfunction.
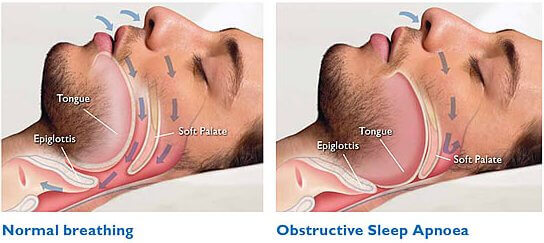
Pathophysiology: What Happens During an Apneic Episode?
The collapse of the pharyngeal airway during sleep is the hallmark of OSA. This obstruction occurs due to the relaxation of the upper airway muscles, particularly during rapid eye movement (REM) sleep, leading to airflow cessation despite ongoing respiratory effort.
Major Risk Factors for Obstructive Sleep Apnea
Anatomical and Physical Risk Factors
- Obesity: Excess soft tissue around the neck increases airway collapsibility
- Large neck circumference (>17 inches in men, >16 inches in women)
- Craniofacial abnormalities: Retrognathia, enlarged tonsils or adenoids
- Nasal congestion or obstruction
Demographic and Genetic Factors
- Age: Higher prevalence in individuals over 40
- Gender: Males are more frequently affected than females
- Family history: Genetic predisposition plays a role
Lifestyle and Comorbidities
- Alcohol or sedative use: Leads to greater muscle relaxation
- Smoking: Increases airway inflammation and fluid retention
- Endocrine disorders: Hypothyroidism and acromegaly are associated with OSA
Key Symptoms and Clinical Features
Nighttime Symptoms
- Loud, chronic snoring
- Observed apneas or gasping during sleep
- Restless sleep and frequent awakenings
- Nocturia (frequent urination at night)
Daytime Symptoms
- Excessive daytime sleepiness (EDS)
- Morning headaches
- Difficulty concentrating and impaired memory
- Mood disturbances, such as irritability or depression
Complications and Long-Term Effects
Untreated OSA increases the risk of serious health consequences:
- Hypertension and cardiac arrhythmias
- Stroke, myocardial infarction, and heart failure
- Type 2 diabetes due to insulin resistance
- Cognitive decline and increased risk of Alzheimer’s disease
- Workplace and motor vehicle accidents due to impaired alertness
Diagnosis: How Obstructive Sleep Apnea Syndrome Is Confirmed
Polysomnography (Sleep Study)
In-laboratory polysomnography is the gold standard for diagnosing OSA. It records:
- Airflow and respiratory effort
- Oxygen saturation levels
- Electroencephalography (EEG) for sleep staging
- Electrooculography (EOG) and electromyography (EMG)
Apnea-Hypopnea Index (AHI)
The AHI quantifies OSA severity:
| AHI Score | Severity |
|---|---|
| 5–14 | Mild OSA |
| 15–29 | Moderate OSA |
| ≥30 | Severe OSA |
Home Sleep Apnea Testing (HSAT)
Suitable for patients with high clinical suspicion, HSAT is a simplified diagnostic tool used at home to monitor breathing and oxygen levels during sleep.
Management and Treatment of Obstructive Sleep Apnea
Lifestyle Modifications
- Weight loss: Reduces the severity or eliminates OSA in overweight individuals
- Positional therapy: Encourages sleeping on the side rather than on the back
- Avoidance of alcohol and sedatives before bedtime
- Smoking cessation to reduce airway inflammation
Continuous Positive Airway Pressure (CPAP) Therapy
CPAP is the first-line treatment for moderate to severe OSA. It delivers a continuous stream of pressurized air to keep the airway open.
Benefits include:
- Reduced AHI and improved oxygenation
- Improved sleep quality and daytime function
- Lowered blood pressure and cardiovascular risk
Alternative Positive Airway Pressure Devices
- Bi-level Positive Airway Pressure (BiPAP): For patients intolerant to CPAP or with central apneas
- Auto-titrating CPAP (APAP): Adjusts pressure levels automatically throughout the night
Oral Appliance Therapy
Mandibular advancement devices (MADs) are custom-fitted oral appliances that reposition the jaw to prevent airway collapse. Recommended for mild to moderate OSA or those intolerant to CPAP.
Surgical Interventions
Surgery may be considered when conservative treatments fail.
- Uvulopalatopharyngoplasty (UPPP): Removes excess tissue from the throat
- Maxillomandibular advancement (MMA): Repositions upper and lower jaws forward
- Hypoglossal nerve stimulation: A pacemaker-like device to stimulate tongue movement
- Tonsillectomy/adenoidectomy: Especially effective in pediatric patients
Obstructive Sleep Apnea in Children
Pediatric OSA has unique features and is often due to enlarged tonsils or adenoids. Symptoms may include:
- Snoring, pauses in breathing during sleep
- Behavioral issues: Inattention, hyperactivity
- Poor academic performance
- Failure to thrive in severe cases
Treatment often involves adenotonsillectomy, followed by CPAP or orthodontic interventions if needed.
Preventive Strategies and Long-Term Management
- Routine screening in high-risk populations (e.g., obese patients, hypertensives)
- Long-term CPAP adherence monitoring to ensure therapeutic efficacy
- Regular follow-ups with sleep specialists
- Integrated care involving pulmonologists, ENT specialists, and dentists
Frequently Asked Questions
Q1: Can obstructive sleep apnea be cured permanently?
Mild cases may resolve with weight loss or surgery. Most cases require lifelong management, especially moderate to severe OSA.
Q2: Is snoring always a sign of sleep apnea?
Not all snoring is due to sleep apnea, but habitual loud snoring with gasping or choking should be evaluated for OSA.
Q3: What is the difference between OSA and central sleep apnea?
OSA involves physical airway obstruction, while central sleep apnea results from impaired brain signals to the respiratory muscles.
Q4: How effective is CPAP therapy?
When used consistently, CPAP virtually eliminates apneas, improves sleep quality, and significantly reduces long-term health risks.
Q5: What are the signs of poor CPAP adherence?
Persistent fatigue, mask discomfort, dry mouth, or waking with the device removed are signs that warrant reassessment of therapy settings.
Obstructive Sleep Apnea Syndrome is a prevalent but often underdiagnosed condition with significant health implications. Prompt recognition, comprehensive diagnostic evaluation, and tailored management strategies—including CPAP, lifestyle modifications, and surgical options—are crucial to improving patient outcomes. By adopting a multidisciplinary and evidence-based approach, we can significantly reduce the disease burden and restore quality sleep and life to those affected by OSA.