Obstructive pulmonary disease is a chronic respiratory disorder characterized by airflow limitation due to airway obstruction. This limitation is typically progressive and not fully reversible, significantly impacting pulmonary function and quality of life. The term most commonly refers to Chronic Obstructive Pulmonary Disease (COPD), which includes both chronic bronchitis and emphysema. Accurate diagnosis, early intervention, and comprehensive disease management are essential to prevent complications and improve outcomes.
Pathophysiology of Airflow Obstruction
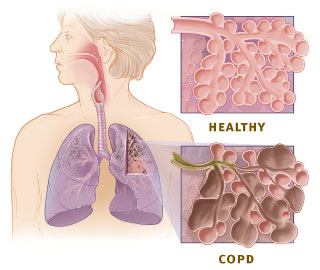
Obstructive pulmonary disease arises from chronic inflammation of the airways, parenchyma, and pulmonary vasculature. This leads to narrowing of the airways, destruction of alveolar walls, mucus hypersecretion, and loss of elastic recoil, all contributing to reduced expiratory airflow.
Major Types of Obstructive Pulmonary Disease
Chronic Obstructive Pulmonary Disease (COPD)
COPD encompasses two main pathological entities:
- Chronic Bronchitis: Defined clinically by a productive cough lasting at least three months over two consecutive years.
- Emphysema: Characterized by destruction of alveolar walls, leading to permanently enlarged airspaces and impaired gas exchange.
Asthma (Chronic Obstructive Variant)
Though traditionally separate, persistent asthma with irreversible airflow limitation may overlap with COPD in some patients.
Bronchiectasis
A form of irreversible bronchial dilation due to chronic infection and inflammation, leading to chronic productive cough and mucopurulent sputum.
Cystic Fibrosis
A genetic disorder causing thick, sticky mucus that obstructs airways, leading to chronic infection, bronchiectasis, and progressive lung damage.
Causes and Risk Factors
Environmental and Lifestyle Factors
- Cigarette smoking: The most significant risk factor for COPD.
- Air pollution: Indoor and outdoor pollutants exacerbate airway inflammation.
- Occupational exposure: Dust, fumes, and chemicals in the workplace.
Genetic Predisposition
- Alpha-1 antitrypsin deficiency: A rare but important genetic cause of early-onset emphysema.
Infections
- Recurrent respiratory infections during childhood can impair lung development and predispose to chronic airway obstruction.
Clinical Presentation and Symptoms
Common Signs and Symptoms
- Dyspnea (shortness of breath), especially during exertion
- Chronic cough, often productive in chronic bronchitis
- Wheezing and chest tightness
- Increased sputum production
- Fatigue and reduced exercise tolerance
Advanced Disease Features
- Barrel-shaped chest due to hyperinflation
- Cyanosis (bluish skin due to low oxygen)
- Polycythemia as a compensatory response
- Pulmonary hypertension and right-sided heart failure (cor pulmonale)
Diagnostic Evaluation
Pulmonary Function Tests (PFTs)
Spirometry is the cornerstone of diagnosis.
- Forced Expiratory Volume in 1 second (FEV1): Markedly reduced
- FEV1/FVC ratio < 0.70 confirms airflow obstruction
- Post-bronchodilator spirometry helps distinguish from asthma
Imaging Studies
- Chest X-ray: May show hyperinflation, flattened diaphragm
- High-Resolution CT (HRCT): Essential for detecting emphysematous changes or bronchiectasis
Laboratory Investigations
- Arterial Blood Gases (ABG): Indicate hypoxemia or hypercapnia
- Alpha-1 Antitrypsin levels in young, non-smoking patients
- Sputum cultures in infectious exacerbations
Treatment Strategies for Obstructive Pulmonary Disease
Lifestyle Modifications
- Smoking cessation: The most effective intervention to slow disease progression
- Vaccinations: Influenza and pneumococcal vaccines reduce exacerbation risk
- Nutritional support and physical activity: Improve overall health status
Pharmacologic Therapy
Bronchodilators
- Short-acting beta-agonists (SABAs): Albuterol for immediate relief
- Long-acting beta-agonists (LABAs) and anticholinergics: Maintain airway patency
Inhaled Corticosteroids (ICS)
- Used in combination with bronchodilators for patients with frequent exacerbations
Phosphodiesterase-4 Inhibitors
- Roflumilast reduces inflammation in severe COPD with chronic bronchitis
Mucolytics
- Aid in sputum clearance in patients with excessive mucus production
Pulmonary Rehabilitation
Structured programs including exercise training, education, and behavior change improve exercise capacity and reduce hospitalizations.
Oxygen Therapy
Long-term oxygen therapy is indicated in patients with chronic hypoxemia (PaO2 < 55 mmHg or SpO2 < 88%).
Surgical Interventions
- Lung volume reduction surgery (LVRS): For upper-lobe predominant emphysema
- Lung transplantation: In select end-stage patients
- Bullectomy: Removal of large bullae that impair breathing mechanics
Prognosis and Disease Progression
The prognosis of obstructive pulmonary disease depends on:
- Severity of airflow limitation (as classified by GOLD stages)
- Frequency of exacerbations
- Presence of comorbidities
- Patient adherence to treatment
Without intervention, COPD progresses irreversibly, but with optimal care, exacerbations can be minimized, and quality of life can be preserved for years.
Obstructive vs. Restrictive Pulmonary Disease
Understanding the distinction between obstructive and restrictive lung diseases is essential in diagnostic evaluation.
| Parameter | Obstructive Pulmonary Disease | Restrictive Pulmonary Disease |
|---|---|---|
| FEV1/FVC Ratio | Decreased (<70%) | Normal or increased |
| Lung Volumes | Increased (air trapping) | Decreased (restricted expansion) |
| Example Conditions | COPD, asthma, bronchiectasis | Pulmonary fibrosis, sarcoidosis |
| Primary Problem | Airflow limitation | Decreased lung compliance |
Frequently Asked Questions
Q1: Is COPD the same as obstructive pulmonary disease?
COPD is the most common form of obstructive pulmonary disease but is not the only type. Bronchiectasis, asthma, and cystic fibrosis also fall under the umbrella of obstructive lung diseases.
Q2: Can obstructive pulmonary disease be cured?
There is no cure, but symptoms can be managed, progression can be slowed, and quality of life can be significantly improved with appropriate care.
Q3: What is the role of spirometry in diagnosis?
Spirometry is essential for confirming airflow limitation and assessing disease severity, which guides treatment decisions.
Q4: Is emphysema always caused by smoking?
While smoking is the most common cause, genetic conditions like alpha-1 antitrypsin deficiency can also lead to emphysema in non-smokers.
Q5: When is oxygen therapy needed?
Oxygen is prescribed in chronic hypoxemia to improve survival, reduce dyspnea, and enhance exercise capacity.
Obstructive pulmonary disease represents a significant global health burden, yet it is manageable with vigilant screening, early diagnosis, and consistent medical intervention. Advances in pharmacological therapies, pulmonary rehabilitation, and personalized treatment protocols have drastically improved patient outcomes. By understanding the underlying pathophysiology and applying a multidisciplinary approach, we can enhance disease control and foster better respiratory health in affected populations.