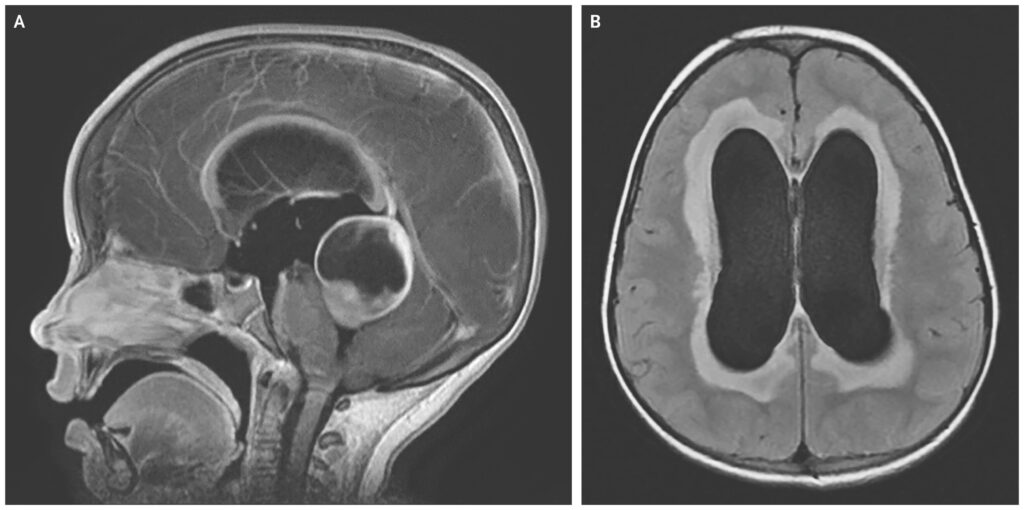
Obstructive hydrocephalus, also known as non-communicating hydrocephalus, is a neurological disorder characterized by a blockage in the normal flow of cerebrospinal fluid (CSF) within the ventricular system of the brain. This obstruction leads to increased intracranial pressure, progressive ventricular dilation, and, if untreated, irreversible brain damage. Understanding the pathophysiology, clinical presentation, diagnostic strategies, and treatment options is vital for timely and effective intervention.
Anatomy and Physiology of CSF Circulation
Cerebrospinal fluid is produced primarily by the choroid plexus within the brain’s ventricles. It flows sequentially through the lateral ventricles, third ventricle, cerebral aqueduct, and fourth ventricle, before exiting into the subarachnoid space and being reabsorbed by arachnoid granulations.
In obstructive hydrocephalus, this flow is impaired at one or more points within the ventricular system, leading to CSF accumulation proximal to the blockage.
Causes of Obstructive Hydrocephalus
Obstructive hydrocephalus can result from various congenital or acquired causes. The location and nature of the obstruction often determine the clinical severity and management approach.
Congenital Causes
- Aqueductal stenosis: Narrowing of the cerebral aqueduct (aqueduct of Sylvius) is the most common congenital cause.
- Chiari malformations: Structural hindbrain abnormalities impeding CSF flow.
- Dandy-Walker malformation: Cystic dilation of the fourth ventricle causing outlet obstruction.
- Neural tube defects: Such as spina bifida, affecting CSF dynamics.
Acquired Causes
- Brain tumors: Ependymomas, medulloblastomas, or astrocytomas blocking CSF pathways.
- Cysts: Arachnoid or colloid cysts compressing ventricular structures.
- Intraventricular hemorrhage: Common in preterm neonates; clotted blood may obstruct CSF pathways.
- Infections: Meningitis leading to inflammatory scarring and obstruction.
- Trauma: Post-traumatic intraventricular clots or swelling impairing flow.
Clinical Presentation and Symptoms
The symptoms of obstructive hydrocephalus vary by age, severity, and the rapidity of onset. Acute obstruction often presents more dramatically than chronic cases.
In Infants
- Rapid head circumference growth
- Bulging fontanelles
- Sunsetting eyes (downward gaze)
- Irritability, poor feeding
- Developmental delays
In Children and Adults
- Headaches, especially in the morning
- Nausea and vomiting
- Papilledema (optic disc swelling)
- Gait disturbances
- Cognitive decline or behavioral changes
- Blurred or double vision
In cases of acute hydrocephalus, patients may present with altered consciousness, which constitutes a neurosurgical emergency.
Diagnostic Evaluation
Neuroimaging
Magnetic Resonance Imaging (MRI) is the gold standard for evaluating ventricular anatomy, identifying obstructive lesions, and assessing CSF flow using phase-contrast techniques.
Computed Tomography (CT) is often used in emergencies due to speed and accessibility, revealing ventricular enlargement and signs of intracranial pressure elevation.
Additional Diagnostic Tools
- Ophthalmologic examination: Detection of papilledema.
- Neuropsychological testing: Evaluation of cognitive impairment in chronic cases.
- Intracranial pressure monitoring: In selected complex cases to guide treatment.
Treatment Options for Obstructive Hydrocephalus
Surgical Interventions
1. Ventriculoperitoneal (VP) Shunt
The most widely used treatment, this procedure involves diverting CSF from the ventricles to the peritoneal cavity using a pressure-regulated valve system.
2. Endoscopic Third Ventriculostomy (ETV)
ETV creates an opening in the floor of the third ventricle to allow CSF to bypass the obstructed aqueduct and flow directly into the subarachnoid space. It is especially effective in aqueductal stenosis.
3. Tumor Resection or Cyst Removal
In cases where a mass lesion causes obstruction, surgical excision may relieve the hydrocephalus permanently.
Medical Management
While not a definitive solution, medications such as acetazolamide or furosemide may be used temporarily to reduce CSF production in acute settings or to bridge the patient to surgery.
Prognosis and Long-Term Outlook
The prognosis of obstructive hydrocephalus depends largely on:
- Underlying cause
- Timeliness of intervention
- Presence of comorbidities
With prompt and appropriate treatment, many patients—especially children—can lead normal lives. However, complications such as shunt malfunction, infection, or neurological sequelae may necessitate long-term follow-up and repeated interventions.
Obstructive vs. Communicating Hydrocephalus
It is crucial to distinguish obstructive hydrocephalus from communicating hydrocephalus, where CSF absorption is impaired but flow is not physically obstructed. The treatment strategies and prognostic considerations differ between these subtypes.
| Feature | Obstructive Hydrocephalus | Communicating Hydrocephalus |
|---|---|---|
| CSF Flow Obstruction | Yes (within ventricles) | No (blockage in absorption pathways) |
| Ventricular Dilatation Pattern | Proximal to obstruction | Generalized |
| Common Causes | Tumors, cysts, congenital anomalies | Meningitis, subarachnoid hemorrhage |
| Treatment | ETV, shunting, lesion excision | Shunting (typically VP shunt) |
Frequently Asked Questions
Q1: Is obstructive hydrocephalus curable?
Yes, many cases can be effectively managed with surgical intervention, particularly when the underlying cause is correctable.
Q2: How urgent is treatment for obstructive hydrocephalus?
Acute obstructive hydrocephalus is a neurosurgical emergency and must be addressed immediately to prevent brain herniation and death.
Q3: Can hydrocephalus recur after treatment?
Yes, particularly in shunt-dependent patients, recurrence due to shunt malfunction or blockage is possible and requires prompt reassessment.
Q4: Is obstructive hydrocephalus hereditary?
Some congenital forms may have genetic components, but many cases are sporadic and not inherited.
Q5: What is the success rate of ETV?
ETV has a high success rate, particularly in patients with aqueductal stenosis and favorable anatomy. Outcomes are better in older children and adults.
Obstructive hydrocephalus represents a critical neurological disorder that demands early recognition, accurate diagnosis, and timely surgical management. Advances in neuroimaging and minimally invasive neurosurgery, such as endoscopic third ventriculostomy, have significantly improved outcomes. Continued research into CSF physiology and hydrocephalus pathogenesis is essential to further refine treatment strategies and reduce long-term morbidity.