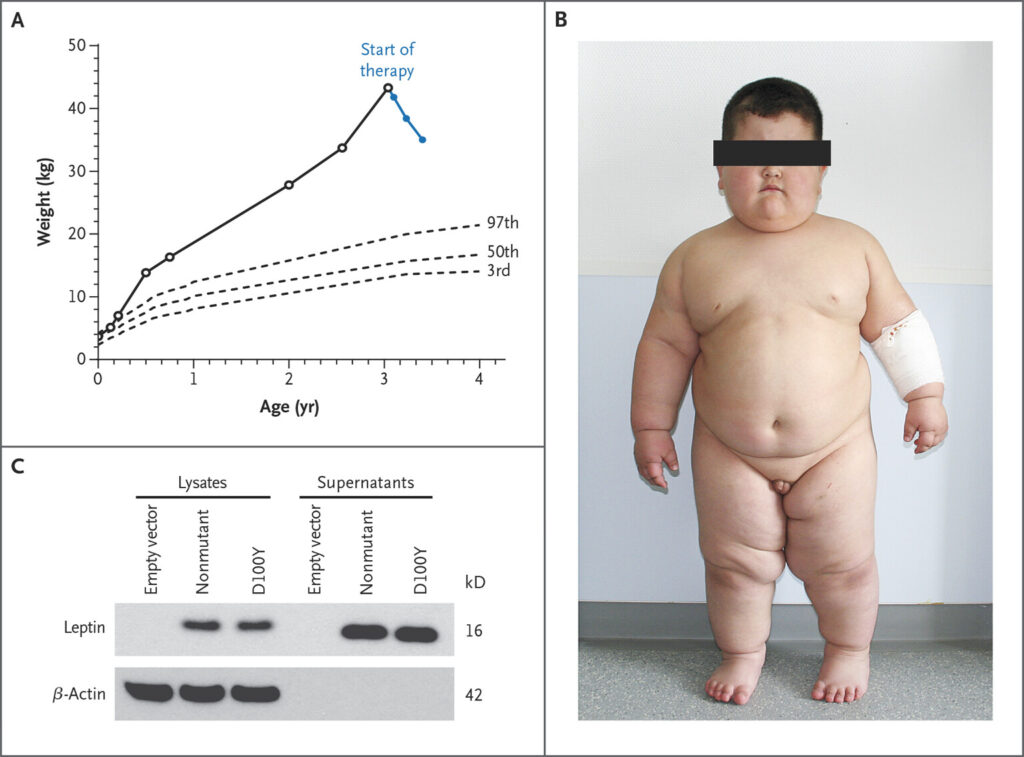
Leptin receptor (LEPR) deficiency is a rare genetic disorder leading to severe, early-onset obesity caused by disruptions in the body’s energy regulation system. As a form of monogenic obesity, LEPR deficiency is linked directly to mutations in a single gene—LEPR—which encodes the receptor for leptin, a hormone critical for regulating appetite and body weight. Individuals affected by LEPR mutations exhibit persistent hunger, impaired satiety, and metabolic dysregulation, requiring targeted diagnostic and therapeutic approaches.
Genetic and Molecular Basis of LEPR Deficiency
LEPR Gene Function and Mutation Impact
The LEPR gene, located on chromosome 1p31, encodes several isoforms of the leptin receptor, including the long form, which is primarily expressed in the hypothalamus. This receptor is essential for mediating leptin’s signal, which suppresses appetite and promotes energy expenditure.
When biallelic mutations (mutations in both copies of the gene) occur in LEPR, the body becomes functionally leptin-resistant—leptin may be present in high quantities, but the receptor cannot respond appropriately. This results in unregulated appetite and rapid weight gain starting in early infancy.
Clinical Characteristics of LEPR Deficiency-Associated Obesity
Key Symptoms and Diagnostic Markers
Patients with LEPR deficiency typically present with:
- Severe hyperphagia beginning in infancy
- Rapid weight gain despite controlled diet
- Early-onset obesity, often by the first year of life
- High circulating leptin levels with no corresponding satiety response
- Delayed puberty or hypogonadotropic hypogonadism
- Mild to moderate immune dysfunction in some cases
Unlike common polygenic obesity, these patients often have a family history suggestive of autosomal recessive inheritance, particularly in consanguineous populations.
Diagnostic Approach to LEPR-Related Obesity
Genetic Testing and Clinical Evaluation
The diagnosis of LEPR deficiency involves:
- Clinical assessment of growth patterns, eating behavior, and early obesity
- Biochemical evaluation, including serum leptin levels
- Targeted genetic testing, ideally via next-generation sequencing (NGS) panels focused on monogenic obesity genes
Confirming biallelic pathogenic mutations in LEPR provides a definitive diagnosis. Early identification is crucial for therapeutic planning and genetic counseling.
Mechanism of Leptin Resistance in LEPR Mutations
Disruption of Hypothalamic Satiety Signaling
Leptin binds to its receptor in the hypothalamus to activate the JAK-STAT pathway, triggering a cascade that promotes satiety and energy expenditure. In LEPR deficiency, this signaling cascade is broken, leading to:
- Continuous hunger signals
- Lack of energy regulation
- Dysregulated glucose and fat metabolism
- Progressive weight gain and associated metabolic disorders
Treatment Strategies for Obesity Due to Leptin Receptor
Limitations of Conventional Therapies
Conventional weight management strategies, such as diet, exercise, and behavioral therapy, are largely ineffective due to the biological inability to sense satiety. Pharmacological treatments used in general obesity often fail to address the core issue of leptin resistance in these patients.
Targeted Therapies and Emerging Treatments
Setmelanotide (MC4R Agonist)
The most promising therapeutic advancement is setmelanotide, an MC4R agonist that bypasses the defective leptin-leptin receptor signaling and directly activates melanocortin pathways involved in satiety.
- FDA-approved for LEPR deficiency-related obesity in patients aged 6 and older
- Demonstrates significant appetite reduction and weight loss in clinical trials
- Requires confirmed genetic diagnosis for prescription
Setmelanotide is not a cure but offers the most direct method for controlling hyperphagia and reducing weight in eligible patients.
Long-Term Management and Monitoring
Multidisciplinary Care for Lifelong Management
Given the chronic and progressive nature of LEPR deficiency, management must be multidisciplinary, involving:
- Endocrinologists for hormonal regulation
- Clinical geneticists for diagnostic and reproductive counseling
- Dietitians to manage nutritional intake within biological limitations
- Psychologists to support behavior management and coping strategies
- Pediatric specialists for growth and pubertal development tracking
Regular monitoring is essential to assess treatment response and prevent complications such as type 2 diabetes, fatty liver disease, and cardiovascular risks.
Prognosis and Quality of Life
With early diagnosis and the availability of targeted therapies, individuals with LEPR deficiency can achieve improved weight control, reduced hunger, and better overall health outcomes. Patient education and family support are key components of effective long-term care, ensuring adherence and emotional resilience.
Summary of Key Clinical Guidelines
- Consider LEPR deficiency in infants or children with early-onset obesity and intense hyperphagia
- Order genetic testing to confirm diagnosis and guide therapy
- Use setmelanotide for eligible patients with biallelic LEPR mutations
- Implement a team-based approach for comprehensive care
- Educate caregivers and patients about the biological nature of the condition
Frequently Asked Questions on Obesity Due to Leptin Receptor
Q1: What is the primary cause of obesity in LEPR deficiency?
The condition is caused by mutations in the LEPR gene, leading to impaired leptin receptor function and resulting in leptin resistance.
Q2: How early does obesity develop in LEPR-deficient individuals?
Symptoms usually begin in infancy, with rapid weight gain and excessive hunger manifesting within the first year.
Q3: Is leptin supplementation effective in LEPR deficiency?
No. Since the receptor is non-functional, increasing leptin levels does not improve symptoms or induce weight loss.
Q4: Can LEPR deficiency be cured?
There is currently no cure, but targeted therapy like setmelanotide offers effective symptom management.
Q5: What is the role of family history in LEPR deficiency?
The disorder is inherited in an autosomal recessive pattern, making family history a significant diagnostic clue, especially in consanguineous families.
Obesity due to leptin receptor (LEPR) deficiency represents a rare but serious form of monogenic obesity. Characterized by insatiable hunger, early-onset weight gain, and hormonal disruption, it challenges conventional treatment paradigms. Advances in genetic diagnostics and targeted therapies such as setmelanotide offer new hope. Through early detection, precision medicine, and a coordinated care approach, we can transform outcomes for patients affected by this debilitating condition.