Bardet-Biedl Syndrome (BBS) is a rare autosomal recessive ciliopathy characterized by multisystemic manifestations, among which obesity is a hallmark. Unlike primary obesity, obesity associated with BBS results from genetic and cellular dysfunctions affecting satiety regulation and energy metabolism. Early diagnosis and tailored intervention are critical for managing the metabolic complications linked to BBS-induced obesity.
Understanding the Genetic Basis of Bardet-Biedl Syndrome
Gene Mutations and Inheritance Patterns
BBS is caused by mutations in at least 26 different genes (BBS1–BBS26), which encode proteins involved in the function and assembly of the primary cilium—an organelle crucial for cellular signaling.
These mutations follow an autosomal recessive inheritance pattern, requiring both alleles to be defective for the phenotype to manifest.
Pathophysiology of Obesity in BBS
Ciliary Dysfunction and Metabolic Dysregulation
The primary cilium plays a vital role in neuroendocrine signaling, particularly within the hypothalamus, which governs appetite control. Disruption of ciliary architecture compromises leptin receptor localization and function, leading to leptin resistance. Consequently, individuals with BBS experience:
- Hyperphagia (increased hunger)
- Reduced energy expenditure
- Early-onset central obesity
- Resistance to conventional weight loss measures
Moreover, ciliary abnormalities also impair insulin signaling and glucose homeostasis, predisposing patients to metabolic syndrome and type 2 diabetes.
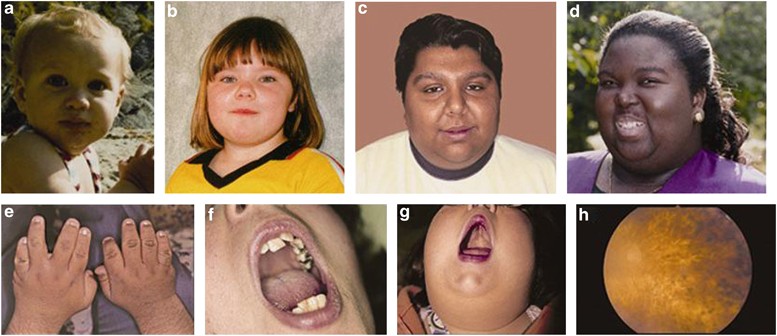
Clinical Features of BBS-Associated Obesity
While obesity is one of the core diagnostic features of BBS, it rarely presents in isolation. Patients often exhibit a combination of the following:
- Truncal obesity with early childhood onset
- Polydactyly (extra digits)
- Retinal dystrophy (progressive vision loss)
- Renal abnormalities (structural and functional)
- Cognitive impairment
- Hypogonadism and genital anomalies
- Developmental delays and behavioral issues
Obesity in BBS often becomes apparent by age five and progresses rapidly without targeted intervention.
Diagnostic Criteria and Early Recognition
The clinical diagnosis of BBS is based on a combination of primary and secondary features. A confirmed diagnosis requires:
- Four primary features, or
- Three primary and two secondary features
Primary Features:
- Rod-cone dystrophy
- Polydactyly
- Obesity
- Learning disabilities
- Renal anomalies
- Hypogonadism
Secondary Features:
- Speech delay
- Ataxia or poor coordination
- Diabetes mellitus
- Congenital heart disease
- Hepatic fibrosis
Genetic testing confirms the diagnosis and identifies the specific BBS gene involved, which can inform prognosis and potential therapeutic response.
Challenges in Weight Management for BBS Patients
Obesity in BBS is not solely lifestyle-driven, making traditional interventions like calorie restriction and increased physical activity less effective. Specific challenges include:
- Persistent hyperphagia due to hypothalamic dysregulation
- Limited physical activity due to visual or developmental impairments
- High risk of insulin resistance and metabolic complications
- Psychological issues such as low self-esteem and behavioral disorders
Thus, weight management in BBS requires a tailored, multidisciplinary approach.
Current and Emerging Treatment Strategies
Nutritional and Behavioral Interventions
- Structured meal plans with portion control
- Family-based behavioral therapy to reinforce healthy habits
- Low glycemic index diets to improve insulin sensitivity
- Scheduled physical activity adapted to mobility and vision challenges
Pharmacological Approaches
- Metformin for insulin resistance
- GLP-1 receptor agonists (e.g., liraglutide) to control appetite and support weight loss
- Setmelanotide, an MC4R agonist, has shown promise in reducing hyperphagia and weight in certain genetic obesity syndromes, including BBS
Surgical Interventions
Bariatric surgery is considered only in adolescents or adults with severe obesity and comorbidities, and where all other interventions have failed.
Role of Genetic Counseling and Family Support
Genetic counseling is essential for families with a history of BBS to understand recurrence risk, inheritance patterns, and available prenatal testing options. Furthermore, caregivers play a vital role in enforcing dietary restrictions, managing medications, and coordinating specialist care.
Long-Term Management and Prognosis
Although BBS is a lifelong condition, proactive management of obesity and its comorbidities can significantly improve life expectancy and quality of life. Ongoing follow-up should include:
- Monitoring of BMI, glucose levels, blood pressure, and renal function
- Regular ophthalmologic and developmental assessments
- Coordination among endocrinologists, nephrologists, geneticists, and dietitians
With early diagnosis and comprehensive care, the metabolic impact of obesity in BBS can be mitigated.
Summary of Key Clinical Recommendations
- Initiate genetic testing for early diagnosis of BBS in children with early-onset obesity and other suggestive features
- Implement multidisciplinary care involving endocrinology, nutrition, and psychology
- Consider pharmacological agents like setmelanotide in genetically appropriate cases
- Monitor for complications such as type 2 diabetes, hypertension, and kidney disease
- Provide ongoing support and education to families and caregivers
Frequently Asked Questions
Q1: Is obesity in Bardet-Biedl syndrome preventable?
While the genetic basis cannot be altered, early intervention and structured management can significantly reduce weight gain and complications.
Q2: What age does obesity typically begin in BBS?
Obesity usually manifests in early childhood, often before the age of five.
Q3: Are weight-loss medications effective in BBS?
Conventional medications have limited efficacy, but targeted therapies like setmelanotide show promise for genetically confirmed cases.
Q4: Does every person with BBS become obese?
Most individuals develop obesity, but severity and progression can vary depending on the specific gene mutation and management.
Q5: Can people with BBS live normal lives?
With comprehensive care, individuals can manage symptoms and lead fulfilling lives, though certain limitations may persist.
Obesity due to Bardet-Biedl Syndrome represents a complex interplay of genetic, neurological, and metabolic dysfunctions. By understanding its unique pathophysiology and tailoring care accordingly, healthcare professionals can significantly improve outcomes for affected individuals. Early genetic diagnosis, multidisciplinary intervention, and emerging targeted therapies offer new hope in the management of syndromic obesity.

