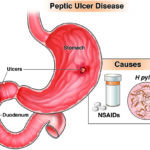
Nsaid induced gastric ulcer: Nonsteroidal anti-inflammatory drugs (NSAIDs) are among the most widely prescribed medications for managing pain and inflammation. However, prolonged or improper NSAID use can compromise gastric mucosal defenses, leading to the development of gastric ulcers. These lesions present a significant burden on healthcare due to their potential to cause serious complications such as bleeding, perforation, and gastric outlet obstruction.

Epidemiology and Risk Demographics
Gastric ulcers resulting from NSAID use are prevalent in both inpatient and outpatient populations. An estimated 10–25% of regular NSAID users develop endoscopically visible gastric ulcers. The incidence is especially high in the elderly, individuals with a prior history of peptic ulcers, and those on concurrent anticoagulant or corticosteroid therapy.
Pathogenesis of NSAID-Induced Gastric Ulcer
Dual Mechanism of Mucosal Damage
NSAIDs induce gastric ulceration through systemic and topical actions:
- Systemic COX Inhibition:
NSAIDs inhibit cyclooxygenase enzymes (COX-1 and COX-2), reducing protective prostaglandins like PGE2 and PGI2 that maintain mucosal blood flow, mucus secretion, and epithelial integrity. COX-1 inhibition is particularly deleterious in the stomach. - Topical Irritant Effect:
The acidic nature of NSAIDs allows them to diffuse into gastric epithelial cells, where they disrupt phospholipid membranes and cause direct cellular injury.
Risk Factors Contributing to Ulceration
Several factors heighten the risk of NSAID-induced gastric ulcers:
- Age > 65 years
- Previous peptic ulcer history
- High-dose or chronic NSAID usage
- Use of anticoagulants, corticosteroids, SSRIs
- Smoking and excessive alcohol use
- Helicobacter pylori infection
Risk stratification is essential for preventing complications in high-risk individuals.
Clinical Manifestations and Symptoms
NSAID-induced gastric ulcers are often silent, particularly in elderly populations. When symptomatic, the following may be noted:
- Epigastric discomfort or burning
- Postprandial fullness and early satiety
- Nausea and intermittent vomiting
- Occult or overt gastrointestinal bleeding (melena, hematemesis)
- Iron-deficiency anemia
A subset of patients may first present with severe complications like ulcer perforation or hemorrhage.
Diagnostic Evaluation
Endoscopy
Upper gastrointestinal endoscopy remains the most definitive diagnostic tool. It provides direct visualization of ulcer characteristics—location, depth, margins—and permits biopsies to exclude malignancy or detect H. pylori.
Additional Diagnostic Tools
- Fecal occult blood test: For suspected chronic bleeding
- Urea breath test or stool antigen test: Detect H. pylori
- Serological testing: Hemoglobin, hematocrit, serum iron for anemia assessment
- Barium studies: Rarely used but may reveal ulcer crater or deformity
Differential Diagnosis
When evaluating gastric ulcers in NSAID users, the following differentials must be considered:
- H. pylori-induced gastric ulcer
- Gastric carcinoma
- Stress-related mucosal disease
- Crohn’s disease involving the stomach
- Zollinger-Ellison syndrome (gastrinoma)
Biopsies during endoscopy are essential to rule out malignancy, especially for ulcers in the gastric body.
Therapeutic Management of NSAID-Induced Gastric Ulcers
Discontinuation of NSAIDs
Whenever feasible, NSAID withdrawal is the first step in management. If discontinuation is not possible, switching to a selective COX-2 inhibitor may offer reduced gastrointestinal toxicity.
Acid Suppression Therapy
Proton Pump Inhibitors (PPIs)
PPIs are the treatment of choice for healing gastric ulcers and preventing recurrence.
- Agents: Omeprazole, Esomeprazole, Lansoprazole, Pantoprazole
- Duration: 6–8 weeks for uncomplicated ulcers
- Mechanism: Profound inhibition of gastric acid secretion via H+/K+ ATPase blockade
H2-Receptor Antagonists
Less effective than PPIs for NSAID-related ulcers but may be used in milder cases or for maintenance therapy.
Cytoprotective Agents
- Misoprostol: A synthetic prostaglandin E1 analog effective in both prevention and treatment. Diarrhea and cramping limit compliance.
- Sucralfate: Forms a protective coating on ulcerated mucosa, supporting healing.
H. pylori Eradication
In patients who test positive for H. pylori, eradication therapy with standard triple or quadruple regimens is essential, regardless of NSAID use, to reduce ulcer recurrence.
Complications and Their Management
NSAID-induced gastric ulcers may result in life-threatening outcomes if not managed effectively:
- Gastrointestinal Bleeding:
Requires endoscopic hemostasis, transfusions, and high-dose intravenous PPI therapy. - Ulcer Perforation:
A surgical emergency. Presents with acute abdomen and free air under diaphragm. - Gastric Outlet Obstruction:
Results from chronic scarring. Managed by endoscopic dilation or surgery.
Early recognition and aggressive management of these complications are paramount in improving outcomes.
Preventive Strategies for High-Risk Patients
Gastroprotection During NSAID Therapy
- Co-prescribe PPIs or misoprostol in patients requiring chronic NSAID use
- Consider COX-2 inhibitors in individuals without cardiovascular risk
- Use the lowest effective NSAID dose for the shortest duration
Monitoring and Lifestyle Modification
- Regular follow-up endoscopies in high-risk populations
- Smoking cessation and avoidance of alcohol
- Avoid concurrent gastrotoxic agents such as corticosteroids or antiplatelets unless absolutely indicated
Summary and Clinical Recommendations
NSAID-induced gastric ulcers represent a preventable but serious condition with potential for fatal complications. Understanding the mechanisms of injury, identifying at-risk individuals, and implementing evidence-based pharmacological therapies are essential for effective management. PPIs remain the cornerstone of both treatment and prevention. When H. pylori is involved, eradication therapy must be integrated into the treatment plan. Clinicians must adopt a proactive approach to ulcer prevention in all NSAID users, particularly those with additional risk factors.