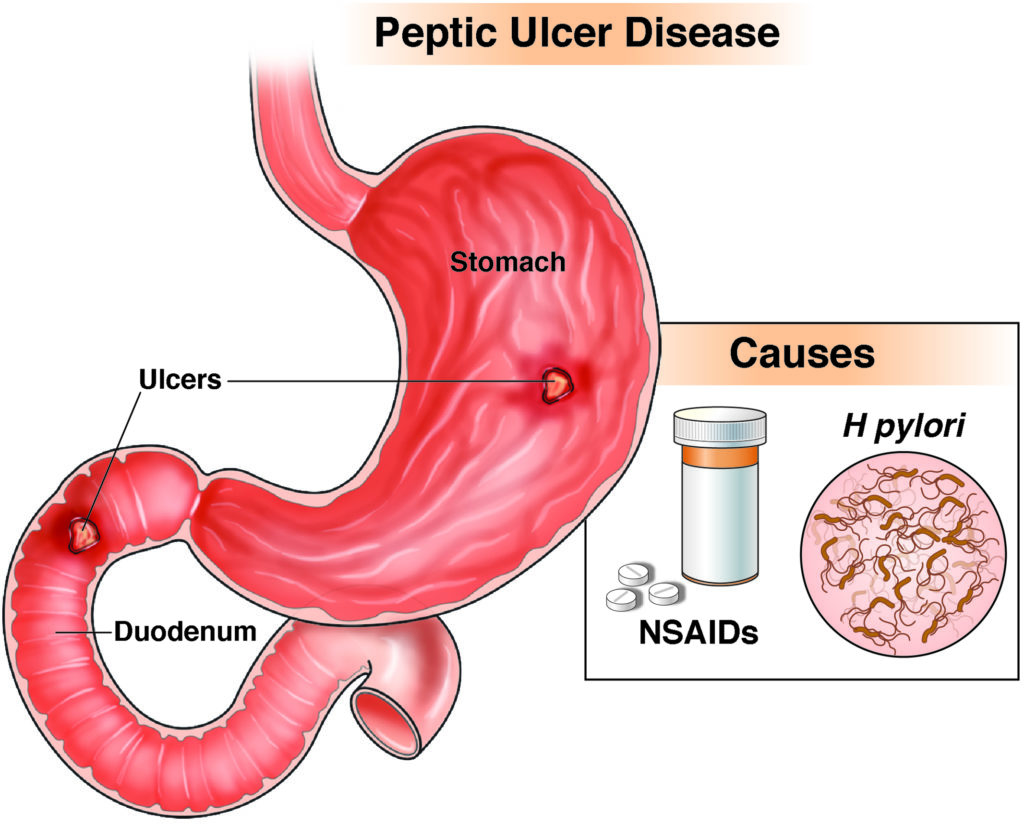
NSAID-induced duodenal ulcers are a critical manifestation of drug-induced gastrointestinal toxicity. Nonsteroidal anti-inflammatory drugs (NSAIDs), widely prescribed for pain and inflammation, disrupt mucosal integrity through systemic and topical mechanisms, leading to ulcer formation in the duodenum. These ulcers, if left untreated, may result in serious complications such as bleeding, perforation, and obstruction.
Epidemiology and Clinical Impact
The prevalence of NSAID-related peptic ulcers, including duodenal ulcers, is significant among chronic users, especially the elderly and those on long-term therapy. Approximately 15–30% of regular NSAID users develop mucosal lesions, with 1–2% experiencing clinically significant ulcers annually. Duodenal ulcers occur more frequently than gastric ulcers among NSAID users without Helicobacter pylori infection.
Pathogenesis of NSAID-Induced Duodenal Ulcer
Mechanisms of Mucosal Injury
NSAIDs compromise the gastrointestinal mucosal defense by:
- Inhibition of Cyclooxygenase (COX) Enzymes: NSAIDs block COX-1 and COX-2, reducing prostaglandin synthesis. COX-1 inhibition impairs mucosal blood flow, mucus secretion, and bicarbonate production, weakening the protective lining of the duodenum.
- Topical Epithelial Damage: NSAIDs cause direct epithelial injury through their acidic nature, disrupting phospholipid membranes of mucosal cells.
- Neutrophil Activation and Free Radical Generation: These contribute to inflammation and oxidative stress, promoting ulceration.
Risk Factors for NSAID-Induced Ulceration
- Age > 60 years
- History of peptic ulcer disease
- Concomitant use of corticosteroids or anticoagulants
- High-dose or multiple NSAID use
- Infection with H. pylori
- Smoking and alcohol consumption
Patients with these risk factors are at substantially higher risk for severe complications such as bleeding and perforation.
Clinical Features and Symptoms
NSAID-induced duodenal ulcers often remain asymptomatic until complications arise. When present, symptoms may include:
- Epigastric pain, typically occurring 1–3 hours after meals and relieved by food
- Bloating and early satiety
- Nausea and occasional vomiting
- Gastrointestinal bleeding (melena or hematemesis)
- Iron-deficiency anemia due to chronic occult bleeding
Diagnostic Modalities
Endoscopy
Upper gastrointestinal endoscopy remains the gold standard for diagnosing duodenal ulcers. It allows direct visualization of ulcer size, location, and depth, and facilitates biopsy if malignancy is suspected.
Non-Endoscopic Investigations
- Fecal occult blood testing: Useful in identifying bleeding ulcers
- Urea breath test or stool antigen test: For detecting concurrent H. pylori infection
- Serum hemoglobin and hematocrit: To assess blood loss
- Serum iron and ferritin levels: For evaluating iron-deficiency anemia
Differential Diagnosis
- H. pylori-induced duodenal ulcer
- Zollinger-Ellison syndrome
- Crohn’s disease
- Eosinophilic gastroenteritis
- Malignancy (rare in the duodenum, but must be ruled out)
Therapeutic Approach and Ulcer Management
Discontinuation of NSAIDs
When clinically feasible, stopping NSAID use is the most effective step in ulcer healing. If cessation is not possible, switching to a selective COX-2 inhibitor may reduce mucosal damage.
Pharmacological Therapy
Proton Pump Inhibitors (PPIs)
PPIs are the cornerstone of treatment and promote ulcer healing by suppressing gastric acid secretion.
- Common agents: Omeprazole, Esomeprazole, Pantoprazole
- Standard course: 4 to 8 weeks of therapy
H2-Receptor Antagonists
Less effective than PPIs but may be used in mild cases or as maintenance therapy.
Mucosal Protective Agents
- Misoprostol: A prostaglandin analog effective in reducing NSAID-related ulceration but associated with gastrointestinal side effects.
- Sucralfate: Forms a protective barrier over the ulcer site.
Treatment of H. pylori Co-infection
When H. pylori is present, eradication therapy must be instituted in addition to acid suppression. Standard triple or quadruple therapy regimens are used.
Complications of NSAID-Induced Duodenal Ulcers
- Hemorrhage: Manifests as hematemesis or melena; may require endoscopic hemostasis or surgical intervention.
- Perforation: A surgical emergency; presents with sudden, severe abdominal pain and signs of peritonitis.
- Gastric Outlet Obstruction: Due to chronic scarring and inflammation.
Preventive Strategies
Risk Stratification
Patients should be assessed for gastrointestinal risk before initiating NSAID therapy. High-risk patients should be prescribed prophylactic measures.
Co-Prescription of Gastroprotective Agents
- PPIs or misoprostol should be prescribed alongside NSAIDs in patients with high GI risk.
- COX-2 inhibitors may be preferred in patients with no cardiovascular risk.
Lifestyle Modifications
- Avoid smoking and excessive alcohol intake
- Limit or eliminate concurrent use of corticosteroids or anticoagulants when possible
- Regular monitoring and follow-up in long-term NSAID users
Summary and Clinical Recommendations
NSAID-induced duodenal ulcers represent a prevalent and preventable clinical problem. Identifying at-risk patients, minimizing NSAID use, and instituting gastroprotective strategies are fundamental in reducing morbidity. Prompt diagnosis through endoscopy and effective pharmacological therapy—primarily with PPIs—are essential for optimal patient outcomes. When H. pylori is present, eradication therapy must accompany ulcer treatment. Clinicians must maintain vigilance for complications and counsel patients on preventive measures to mitigate long-term risks.