Nosocomial Pneumonia Due to Streptococcus pneumoniae: Nosocomial pneumonia, commonly referred to as hospital-acquired pneumonia (HAP), is an infection of the lung parenchyma that occurs 48 hours or more after hospital admission and was not incubating at the time of admission. Among the microbial agents responsible, Streptococcus pneumoniae stands out as a significant etiological agent, especially in non-ventilated patients and in early-onset HAP.
Epidemiology and Risk Factors
Incidence and Mortality
Nosocomial pneumonia remains one of the leading causes of morbidity and mortality among hospitalized patients. Infections caused by S. pneumoniae are associated with a mortality rate ranging from 20% to 50%, particularly in immunocompromised individuals and elderly patients.
Key Risk Factors on Nosocomial Pneumonia Due to Streptococcus pneumoniae
- Advanced age
- Prolonged hospitalization
- Mechanical ventilation (though S. pneumoniae is more common in non-VAP)
- Immunosuppressive therapy or underlying immunodeficiency
- Chronic obstructive pulmonary disease (COPD)
- Aspiration and altered consciousness
Pathogenesis of Pneumococcal Nosocomial Pneumonia
Mechanisms of Infection
The pathogenic mechanism of Streptococcus pneumoniae involves colonization of the oropharyngeal mucosa followed by microaspiration into the lower respiratory tract. In compromised hosts, the bacterium evades the immune system via a polysaccharide capsule that inhibits phagocytosis.
Host Response
Upon reaching the alveoli, pneumococci trigger an inflammatory cascade involving cytokines like IL-1, IL-6, and TNF-α. This leads to alveolar filling with exudates, compromising gas exchange and promoting respiratory symptoms.
Clinical Features
Common Symptoms
- Sudden onset of fever
- Productive cough with purulent sputum
- Dyspnea and pleuritic chest pain
- Hypoxia and tachypnea
Physical Examination
Findings may include bronchial breath sounds, crackles, dullness to percussion, and decreased breath sounds in affected lobes.
Diagnostic Approaches
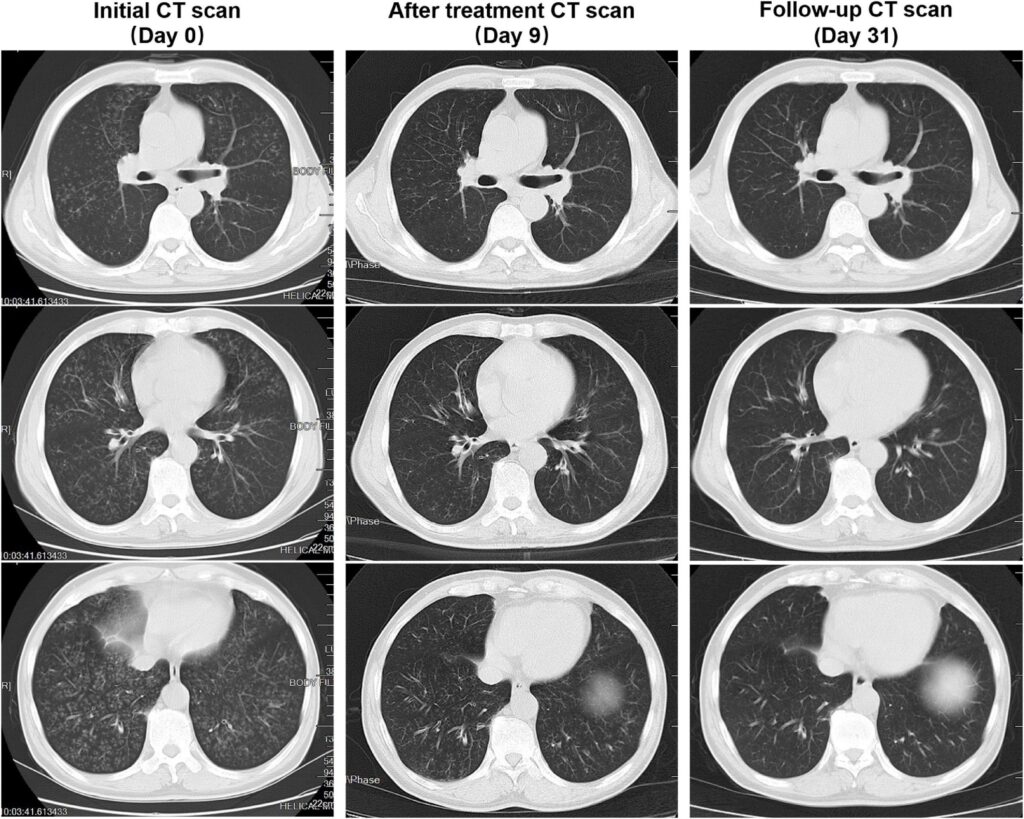
Radiological Imaging
A chest X-ray or CT scan typically reveals new or progressive infiltrates consistent with pneumonia, although differentiation from other causes of lung opacities in hospitalized patients can be challenging.
Microbiological Testing
- Sputum Gram stain and culture: Presence of gram-positive diplococci.
- Blood cultures: Positive in up to 25% of cases.
- Urinary antigen testing: High sensitivity and specificity for S. pneumoniae.
- Bronchoalveolar lavage (BAL) and protected specimen brush (PSB): Useful in intubated patients.
Antibiotic Resistance in Streptococcus pneumoniae
Mechanisms of Resistance
- Altered penicillin-binding proteins (PBPs)
- Efflux pumps and macrolide resistance genes (erm, mef)
- Fluoroquinolone resistance mutations (parC, gyrA)
Prevalence
The global rise in multidrug-resistant (MDR) strains of S. pneumoniae presents a critical challenge, particularly in regions with high antibiotic usage.
Treatment Strategies
Empirical Therapy
Initial treatment should cover S. pneumoniae and other common nosocomial pathogens:
- Preferred agents: Third-generation cephalosporins (e.g., ceftriaxone), respiratory fluoroquinolones (e.g., levofloxacin), or beta-lactam/macrolide combinations.
- For MDR strains: Vancomycin or linezolid may be necessary.
- Duration: Typically 7 to 14 days, based on clinical response.
De-escalation
Once the pathogen is identified and sensitivities are known, narrowing antibiotic coverage minimizes resistance development and adverse effects.
Prevention and Control
Vaccination
- Pneumococcal conjugate vaccine (PCV13) and polysaccharide vaccine (PPSV23) are essential for high-risk individuals.
- Healthcare workers should be immunized to reduce transmission risks.
Infection Control Measures
- Adherence to hand hygiene
- Use of personal protective equipment (PPE)
- Avoiding unnecessary mechanical ventilation
- Elevating the head of the bed in ventilated patients
- Regular oral care with chlorhexidine in ICUs
Prognosis and Outcomes
Despite appropriate therapy, nosocomial pneumonia due to S. pneumoniae can result in poor outcomes, especially in patients with comorbidities or delayed treatment. Early recognition, targeted therapy, and supportive care are crucial in improving prognosis.
Nosocomial pneumonia due to Streptococcus pneumoniae represents a significant clinical burden in hospitalized patients. Understanding its pathogenesis, resistance trends, and effective management protocols is vital for reducing mortality and improving patient outcomes. Continued surveillance, judicious antibiotic use, and preventive strategies including vaccination remain the cornerstone of control efforts.