Bacteroides empyema refers to a purulent infection within the pleural cavity, primarily caused by bacteria of the genus Bacteroides. These are anaerobic, gram-negative bacilli commonly found in the human gastrointestinal tract. Despite their symbiotic roles in maintaining gut health, Bacteroides species can become opportunistic pathogens, especially when translocated to sterile sites, such as the pleural space.
Empyema caused by Bacteroides is associated with significant morbidity and requires prompt diagnosis and treatment. This article delves into the etiology, pathogenesis, clinical presentation, diagnostic methods, and therapeutic approaches for managing this condition.
Etiology and Pathogenesis
Role of Bacteroides Species
Key Bacteroides species implicated in empyema include:
- Bacteroides fragilis: The most clinically significant species, known for its virulence and resistance mechanisms.
- Bacteroides thetaiotaomicron: Typically part of the gut microbiota but pathogenic in pleural infections.
- Bacteroides vulgatus: Occasionally implicated in anaerobic infections.
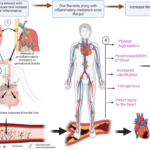
These bacteria enter the pleural cavity through mechanisms such as:
- Contiguous Spread: From intra-abdominal infections like ruptured appendicitis or diverticulitis.
- Hematogenous Dissemination: Via the bloodstream in systemic infections.
- Direct Inoculation: Following thoracic procedures, trauma, or penetrating injuries.
Pathophysiological Mechanisms
Once in the pleural cavity, Bacteroides species proliferate in the anaerobic environment, releasing enzymes and toxins that:
- Induce tissue necrosis and inflammation.
- Facilitate pus formation.
- Disrupt local immune responses.
Clinical Presentation
Patients with bacteroides empyema may present with symptoms such as:
- Respiratory Symptoms: Pleuritic chest pain, dyspnea, and cough (productive or nonproductive).
- Systemic Manifestations: Fever, chills, malaise, and weight loss.
- Signs of Pleural Effusion: Dullness to percussion, decreased breath sounds, and reduced chest wall expansion on the affected side.
Complications can include septicemia, lung abscess, and bronchopleural fistula.
Diagnostic Approach
Clinical Evaluation
Initial evaluation involves a thorough history and physical examination. Risk factors such as recent abdominal infections, surgeries, or trauma should raise suspicion.
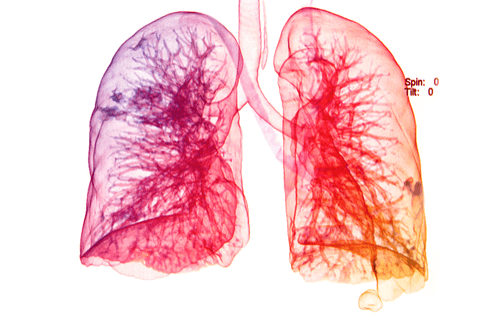
Imaging Studies
- Chest X-ray: Reveals pleural effusion, typically unilateral.
- Ultrasound: Helps identify loculated effusions and guides thoracentesis.
- CT Scan: Provides detailed imaging of the pleural space and adjacent structures.
Laboratory Tests
- Pleural Fluid Analysis:
- Appearance: Purulent.
- Biochemistry: Low glucose, low pH, and elevated lactate dehydrogenase (LDH).
- Microbiology: Gram stain and anaerobic culture to confirm Bacteroides species.
- Blood Tests:
- Leukocytosis with a left shift.
- Elevated inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR).
Treatment Strategies
Medical Management
- Antibiotic Therapy:
- Empiric coverage: Broad-spectrum antibiotics with anaerobic coverage (e.g., piperacillin-tazobactam or carbapenems).
- Tailored therapy: Based on culture and sensitivity results.
- Duration: Typically 4-6 weeks, depending on clinical response.
- Supportive Care:
- Oxygen therapy for hypoxia.
- Analgesics for pleuritic pain.
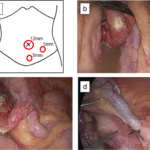
Interventional Approaches
- Thoracentesis: Diagnostic and therapeutic aspiration of pleural fluid.
- Chest Tube Drainage: Placement of a chest tube for continuous drainage of pus.
- Surgical Intervention:
- Video-assisted thoracoscopic surgery (VATS) for decortication.
- Open thoracotomy in severe or refractory cases.
Prevention and Prognosis
Prevention
- Early recognition and treatment of intra-abdominal infections.
- Adherence to sterile techniques during surgical procedures.
Prognosis
With prompt and adequate treatment, the prognosis of bacteroides empyema is favorable. Delayed diagnosis or inadequate drainage can lead to chronic empyema, systemic sepsis, or death.
Bacteroides empyema is a serious but treatable condition requiring a multidisciplinary approach. Early diagnosis through clinical suspicion, imaging, and laboratory testing is critical. Comprehensive management, including appropriate antibiotics and drainage procedures, ensures favorable outcomes for most patients.