Neuropathic pain is a debilitating consequence of spinal cord injury (SCI), affecting a significant proportion of patients. It arises due to damage to the spinal cord and nerves, leading to abnormal pain processing. Unlike nociceptive pain, which results from direct tissue damage, neuropathic pain is caused by maladaptive nerve signaling. This condition significantly impacts quality of life, mobility, sleep, and mental health.
Understanding the mechanisms of neuropathic pain in SCI is crucial for early diagnosis and effective management, as it is often resistant to conventional pain treatments.
Pathophysiology of Neuropathic Pain in Spinal Cord Injury
Neuropathic pain in SCI results from structural and functional changes in the nervous system. The disruption of spinal pathways leads to abnormal pain perception.
- Peripheral nerve damage leads to increased excitability and spontaneous firing of pain signals.
- Central sensitization occurs due to persistent nociceptive input, amplifying pain responses.
- Glial cell activation contributes to neuroinflammation, intensifying pain processing.
- Loss of inhibitory control at the spinal level results in heightened pain transmission.
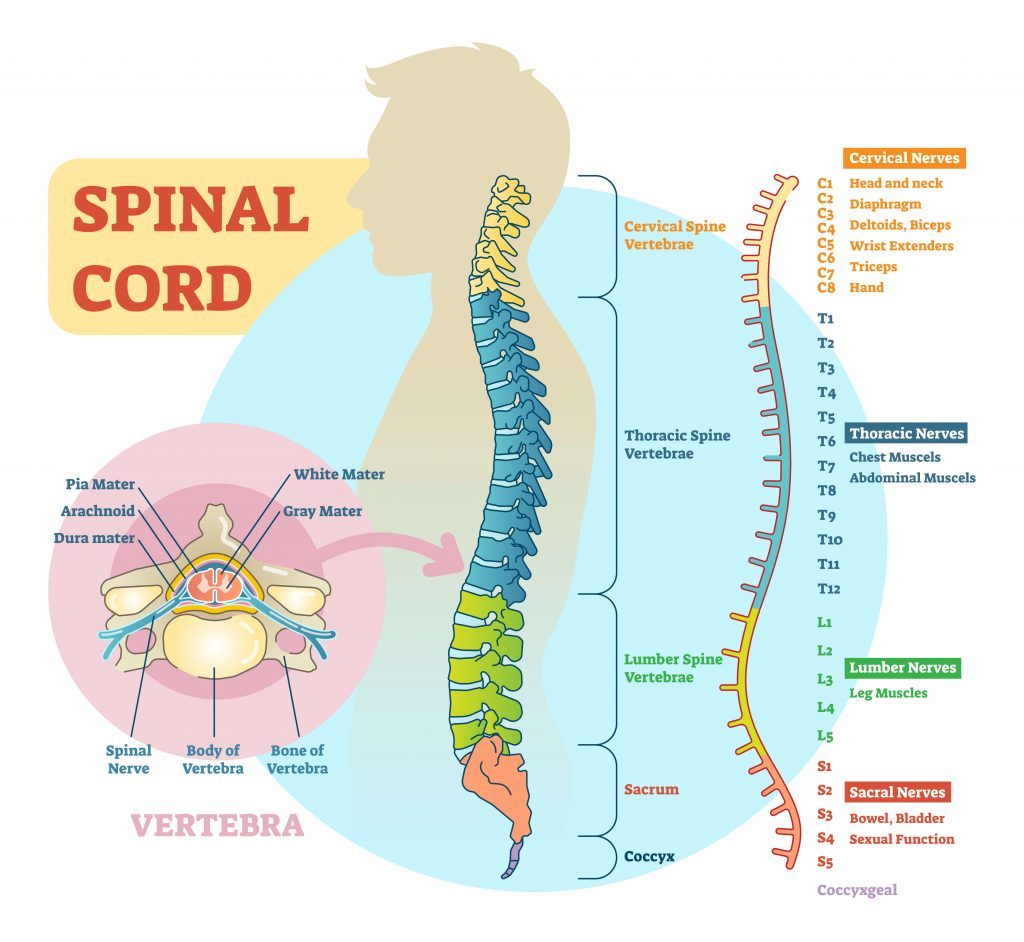
Types of Neuropathic Pain in Spinal Cord Injury
Neuropathic pain in SCI can be classified into different types based on pain origin and characteristics.
1. At-Level Neuropathic Pain
- Occurs at the site of spinal cord injury.
- Described as burning, tingling, or electric shock-like pain.
- Caused by damage to nerve roots or spinal cord segments.
2. Below-Level Neuropathic Pain
- Manifests below the level of the injury in areas with sensory impairment.
- Common in complete and incomplete SCI.
- Associated with central sensitization and loss of inhibitory control.
3. Segmental Pain
- Occurs in the dermatomes adjacent to the injured spinal segment.
- Due to nerve root compression or damage.
Causes and Risk Factors
Several factors contribute to the development and persistence of neuropathic pain in SCI.
1. Nerve Damage and Maladaptive Plasticity
- Injury-induced changes in neural circuits alter pain processing.
- Ectopic nerve activity leads to spontaneous pain generation.
2. Inflammation and Glial Activation
- Activation of microglia and astrocytes contributes to chronic neuroinflammation.
- Increased pro-inflammatory cytokines (TNF-α, IL-1β, IL-6) enhance pain sensitivity.
3. Psychological and Environmental Factors
- Depression, anxiety, and stress amplify pain perception.
- Sleep disturbances and immobility worsen neuropathic symptoms.
Symptoms in SCI
Neuropathic pain presents with diverse sensory abnormalities.
1. Sensory Symptoms
- Burning or stabbing pain – Persistent, localized pain.
- Electric shock sensations – Sudden jolts of pain.
- Tingling and numbness – Abnormal sensations in affected areas.
2. Stimulus-Evoked Pain
- Allodynia – Pain from non-painful stimuli (e.g., light touch).
- Hyperalgesia – Exaggerated pain response to mild stimuli.
3. Autonomic and Motor Symptoms
- Muscle spasms – Involuntary contractions due to nerve dysfunction.
- Skin hypersensitivity – Increased sensitivity to heat and cold.
Diagnosis
Accurate diagnosis is essential for targeted treatment.
1. Clinical Assessment
- Detailed pain history – Onset, duration, triggers, and intensity.
- Neurological examination – Sensory and motor function testing.
- Pain questionnaires – Neuropathic Pain Scale (NPS), McGill Pain Questionnaire (MPQ).
2. Diagnostic Tests
- MRI and CT scans – Evaluate spinal cord damage.
- Electromyography (EMG) – Assesses nerve function.
- Quantitative sensory testing (QST) – Measures pain thresholds.
Treatment Strategies for Neuropathic Pain in SCI
A multimodal approach is essential to manage SCI-related neuropathic pain effectively.
1. Pharmacological Treatments
First-Line Medications
- Anticonvulsants (Gabapentin, Pregabalin) – Reduce nerve excitability.
- Tricyclic Antidepressants (Amitriptyline, Nortriptyline) – Block pain transmission.
- Serotonin-Norepinephrine Reuptake Inhibitors (Duloxetine, Venlafaxine) – Modulate pain pathways.
Second-Line Medications
- Opioids (Tramadol, Tapentadol) – Reserved for severe, refractory pain.
- Topical Agents (Lidocaine patches, Capsaicin cream) – Provide localized pain relief.
2. Interventional Procedures
- Spinal Cord Stimulation (SCS) – Electrical impulses to modulate pain signals.
- Intrathecal Drug Delivery – Direct administration of pain-relief medications.
- Dorsal Root Ganglion (DRG) Stimulation – Targets nerve roots for pain control.
3. Physical and Psychological Therapies
- Transcutaneous Electrical Nerve Stimulation (TENS) – Non-invasive nerve stimulation.
- Cognitive Behavioral Therapy (CBT) – Addresses pain-related distress.
- Acupuncture and Mindfulness Therapy – Complementary pain management techniques.
Complications and Long-Term Impact
If left untreated, neuropathic pain in SCI can lead to:
✅ Chronic disability – Reduced mobility and function.
✅ Psychological distress – Depression, anxiety, and emotional exhaustion.
✅ Sleep disturbances – Disrupted rest patterns.
✅ Dependence on medications – Increased risk of drug tolerance and side effects.
Prevention and Long-Term Management
1. Preventive Strategies
- Early rehabilitation to maintain mobility and prevent secondary complications.
- Regular monitoring for signs of nerve dysfunction.
- Lifestyle modifications including exercise, nutrition, and stress management.
2. Long-Term Management Approaches
- Personalized pain management plans tailored to individual needs.
- Integrative therapies combining medications, therapy, and interventional procedures.
- Patient education to enhance self-management strategies.
Neuropathic pain in spinal cord injury is a chronic and life-altering condition requiring a comprehensive treatment approach. Advances in pharmacological, interventional, and rehabilitative therapies offer effective pain relief, but multidisciplinary care remains essential. Early intervention and personalized treatment significantly improve the prognosis and enhance the quality of life for individuals living with SCI-related neuropathic pain.