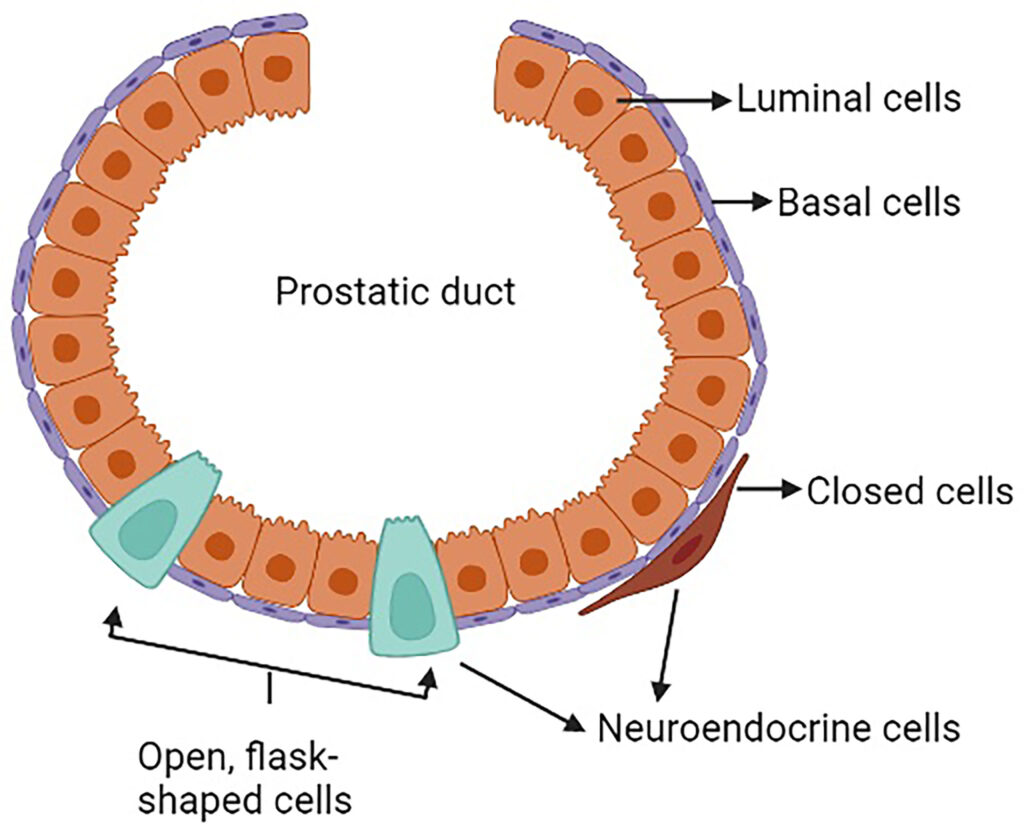
Neuroendocrine prostate carcinoma (NEPC) is a rare and aggressive subtype of prostate cancer that arises from neuroendocrine cells within the prostate. Unlike conventional adenocarcinoma, which is androgen-dependent, NEPC is typically androgen-independent, making it resistant to traditional hormonal therapies. NEPC accounts for less than 2% of primary prostate cancers but can emerge as a treatment-resistant variant in advanced prostate cancer cases following androgen deprivation therapy (ADT). It is characterized by rapid progression, high metastatic potential, and poor prognosis.
Pathogenesis and Development of NEPC
1. Cellular Origin and Molecular Pathways
NEPC arises through transdifferentiation of prostate adenocarcinoma cells or from de novo differentiation of neuroendocrine cells. The transition to NEPC is driven by:
- Loss of Androgen Receptor (AR) expression – Conventional therapies targeting androgen signaling become ineffective.
- Overexpression of neuroendocrine markers – Increased expression of chromogranin A (CgA), synaptophysin (SYP), and neuron-specific enolase (NSE).
- Genetic and epigenetic alterations – Mutations in RB1, TP53, and PTEN contribute to cancer progression.
2. Transition from Prostate Adenocarcinoma to NEPC
NEPC can develop from conventional prostate adenocarcinoma, particularly after prolonged androgen deprivation therapy (ADT).
Clinical Presentation and Symptoms
1. Common Symptoms of NEPC
- Rapidly progressing urinary symptoms – Urinary obstruction, dysuria, and hematuria.
- Bone pain and fractures – Due to early metastasis to bones.
- Neurological symptoms – Caused by spinal cord compression from vertebral metastases.
- Paraneoplastic syndromes – Rare but may include Cushing’s syndrome due to ectopic ACTH secretion.
2. Differences Between NEPC and Adenocarcinoma
| Feature | Neuroendocrine Prostate Carcinoma (NEPC) | Prostate Adenocarcinoma |
|---|---|---|
| Androgen Receptor (AR) Expression | Negative | Positive |
| PSA Levels | Often Normal | Elevated |
| Metastatic Potential | High, rapid spread to liver and brain | Primarily to bones |
| Response to ADT | Resistant | Sensitive |
| Neuroendocrine Markers | Chromogranin A, Synaptophysin | Absent |
Diagnosis of Neuroendocrine Prostate Carcinoma
1. Biomarker Testing
- Low Prostate-Specific Antigen (PSA) levels despite aggressive disease.
- Elevated neuroendocrine markers: Chromogranin A (CgA), Synaptophysin (SYP), Neuron-Specific Enolase (NSE).
- Serum lactate dehydrogenase (LDH) and carcinoembryonic antigen (CEA) may also be elevated.
2. Imaging Studies
- Multiparametric MRI (mpMRI): Helps detect intraprostatic and metastatic lesions.
- PET-CT with Gallium-68 DOTATATE: Superior for detecting neuroendocrine tumors (NETs).
- Bone scans: Essential for identifying skeletal metastases.
3. Histopathological Examination
- Biopsy with immunohistochemistry (IHC): Confirms NEPC by detecting chromogranin A, synaptophysin, and neuron-specific enolase.
- High Ki-67 proliferation index: Suggests aggressive tumor growth.
Treatment Strategies for NEPC
1. Chemotherapy as First-Line Treatment
Since NEPC does not respond to androgen deprivation therapy, chemotherapy is the primary treatment.
- Platinum-based regimens (Cisplatin or Carboplatin + Etoposide): Standard treatment for small cell neuroendocrine carcinoma (SCNC).
- Docetaxel + Carboplatin: Used for mixed adenocarcinoma-NEPC cases.
2. Targeted Therapy and Immunotherapy
- PARP inhibitors (Olaparib, Rucaparib): Beneficial in patients with BRCA mutations.
- PD-L1/PD-1 inhibitors (Pembrolizumab): Show promise in immune checkpoint blockade therapy.
3. Radiation Therapy
- Used for localized NEPC or palliative treatment in bone and brain metastases.
- Whole-brain radiation therapy (WBRT): Recommended for brain metastases.
4. Surgery in Selected Cases
- Radical prostatectomy only considered in early-stage localized disease (rare).
Prognosis and Survival Rates
1. Survival Statistics
- Median survival of de novo NEPC: 9-13 months due to aggressive behavior.
- Treatment-emergent NEPC (from adenocarcinoma): 12-18 months survival post-diagnosis.
- Localized NEPC with treatment: 5-year survival below 20%.
2. Factors Affecting Prognosis
- Presence of visceral metastases (liver, lungs, brain) worsens survival.
- Response to platinum-based chemotherapy determines progression-free survival.
Prevention and Early Detection
1. Genetic and Molecular Screening
- Regular monitoring of androgen-independent tumors in patients undergoing prolonged ADT.
- Next-generation sequencing (NGS) for identifying mutations linked to NEPC progression.
2. Early Imaging and Biomarker Evaluation
- Patients on androgen deprivation therapy (ADT) should undergo routine MRI and biomarker screening for early signs of NEPC.
Neuroendocrine prostate carcinoma (NEPC) is a rare but highly aggressive form of prostate cancer. It often develops in advanced prostate cancer patients as a treatment-resistant variant. Due to its poor prognosis and high metastatic potential, early detection through biomarkers and imaging is essential. While chemotherapy remains the primary treatment, emerging targeted therapies and immunotherapies offer new hope for patients. Continued research into genetic markers and novel therapeutic approaches is crucial for improving outcomes in NEPC.