A neoplasm of the breast refers to an abnormal and uncontrolled growth of cells within the breast tissue. These neoplasms may be benign (non-cancerous) or malignant (cancerous), with the latter posing significant health risks. Early identification and categorization are crucial for successful management and prognosis.
Classification of Breast Neoplasms
Benign vs. Malignant Neoplasms
- Benign Neoplasms: Non-invasive, typically slow-growing tumors that do not spread. Common types include fibroadenomas, intraductal papillomas, and phyllodes tumors.
- Malignant Neoplasms (Breast Cancer): These tumors are invasive, can metastasize, and include various histological subtypes such as invasive ductal carcinoma and invasive lobular carcinoma.
Primary vs. Secondary Breast Neoplasms
- Primary Breast Neoplasms: Originate within the breast tissue.
- Secondary (Metastatic) Neoplasms: Rare and result from cancers spreading from other organs, such as lung or melanoma.
Types of Benign Breast Neoplasms
Fibroadenoma
- Most common benign breast tumor, especially in women under 30.
- Typically mobile, painless, and firm.
- Hormone-sensitive and may enlarge during pregnancy or hormone therapy.
Phyllodes Tumor
- Rare fibroepithelial tumor; may be benign, borderline, or malignant.
- Can grow rapidly and may recur if not excised completely.
Intraductal Papilloma
- Small, wart-like growths in the milk ducts near the nipple.
- Often associated with nipple discharge.
Types of Malignant Breast Neoplasms
Invasive Ductal Carcinoma (IDC)
- Accounts for 70–80% of all breast cancers.
- Originates in the milk ducts and invades surrounding tissues.
Invasive Lobular Carcinoma (ILC)
- Originates in the milk-producing lobules.
- Often less distinct on imaging and more difficult to detect early.
Ductal Carcinoma In Situ (DCIS)
- Non-invasive form where abnormal cells are confined within the ducts.
- Considered a precursor to invasive cancer.
Triple-Negative Breast Cancer (TNBC)
- Lacks estrogen, progesterone, and HER2 receptors.
- Aggressive and often affects younger women.
HER2-Positive Breast Cancer
- Characterized by overexpression of the HER2 protein.
- Responds well to targeted therapies like trastuzumab.
Risk Factors for Breast Neoplasms
- Gender: Predominantly affects females, though males can develop breast neoplasms.
- Age: Risk increases with age, especially after 50.
- Genetic Mutations: BRCA1 and BRCA2 mutations significantly raise the risk.
- Family History: A close relative with breast cancer increases risk.
- Hormonal Factors: Early menarche, late menopause, and hormone replacement therapy.
- Lifestyle: Alcohol consumption, obesity, and sedentary behavior.
Symptoms and Clinical Signs
- Presence of a breast lump, often hard and immobile in malignancy.
- Nipple discharge, possibly bloody.
- Breast pain or tenderness, although less common in malignancies.
- Skin dimpling, peau d’orange texture, or nipple retraction.
- Swelling in part or all of the breast, with or without a lump.
- Axillary lymphadenopathy—swelling in underarm lymph nodes.
Diagnostic Evaluation
Imaging Studies
- Mammography: First-line imaging for women over 40.
- Ultrasound: Differentiates solid from cystic lesions, ideal for younger women.
- MRI: Highly sensitive; used in high-risk cases or dense breast tissue.
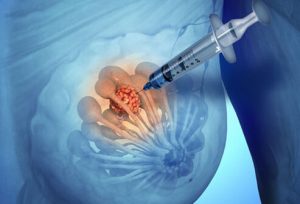
Biopsy Techniques
- Fine Needle Aspiration Cytology (FNAC)
- Core Needle Biopsy
- Excisional Biopsy
Histopathological and immunohistochemical analysis determine tumor subtype, grade, and receptor status (ER, PR, HER2).
Tumor Marker Tests
- Evaluate hormone receptor status (ER/PR)
- HER2/neu gene amplification (via FISH or IHC)
- Ki-67 index for proliferation
Staging of Malignant Breast Neoplasms
Staging follows the TNM classification:
- T (Tumor size)
- N (Lymph node involvement)
- M (Distant metastasis)
| Stage | Description |
|---|---|
| I | Tumor ≤ 2 cm, no lymph node involvement |
| II | Tumor 2–5 cm, possible node involvement |
| III | Tumor > 5 cm or extensive node spread |
| IV | Distant metastasis (bones, liver, lungs) |
Treatment of Breast Neoplasms
Surgical Options
- Lumpectomy: Tumor excision with breast conservation.
- Mastectomy: Total removal of the breast; may include nipple-sparing variants.
- Sentinel Lymph Node Biopsy or Axillary Dissection: To assess spread.
Radiation Therapy
- Often follows breast-conserving surgery.
- Reduces local recurrence risk.
Chemotherapy
- Administered in adjuvant (post-surgery) or neoadjuvant (pre-surgery) settings.
- Common agents: doxorubicin, cyclophosphamide, paclitaxel.
Hormonal Therapy
- Tamoxifen for premenopausal women.
- Aromatase inhibitors (anastrozole, letrozole) for postmenopausal women.
Targeted Therapy
- HER2-positive tumors: Trastuzumab, pertuzumab.
- CDK4/6 inhibitors: For hormone receptor-positive metastatic disease.
- PARP inhibitors: For BRCA-mutated cancers.
Prognosis and Survival Outlook
- Depends on stage at diagnosis, tumor biology, patient age, and overall health.
- Five-year survival rates:
| Type | Survival Rate |
|---|---|
| Localized Breast Cancer | ~99% |
| Regional Spread (Lymph Nodes) | ~86% |
| Distant Metastatic Breast Cancer | ~30% |
| Triple-Negative Breast Cancer | ~77% (localized) |
| HER2-Positive (treated) | Improved with targeted therapy |
Early detection through regular screening drastically improves prognosis.
Preventive Measures and Screening
- Routine mammography after age 40 or earlier in high-risk individuals.
- Self-breast examination and clinical breast exams.
- Genetic counseling and BRCA testing for at-risk populations.
- Lifestyle modification: Weight control, physical activity, reduced alcohol.
Neoplasms of the breast encompass a wide spectrum of pathological conditions from benign tumors to invasive carcinomas. Early identification, precise histopathological classification, and personalized treatment plans significantly enhance patient outcomes. With the advancement of targeted therapies and improved diagnostic techniques, the survival rates and quality of life for individuals with breast neoplasms continue to improve.