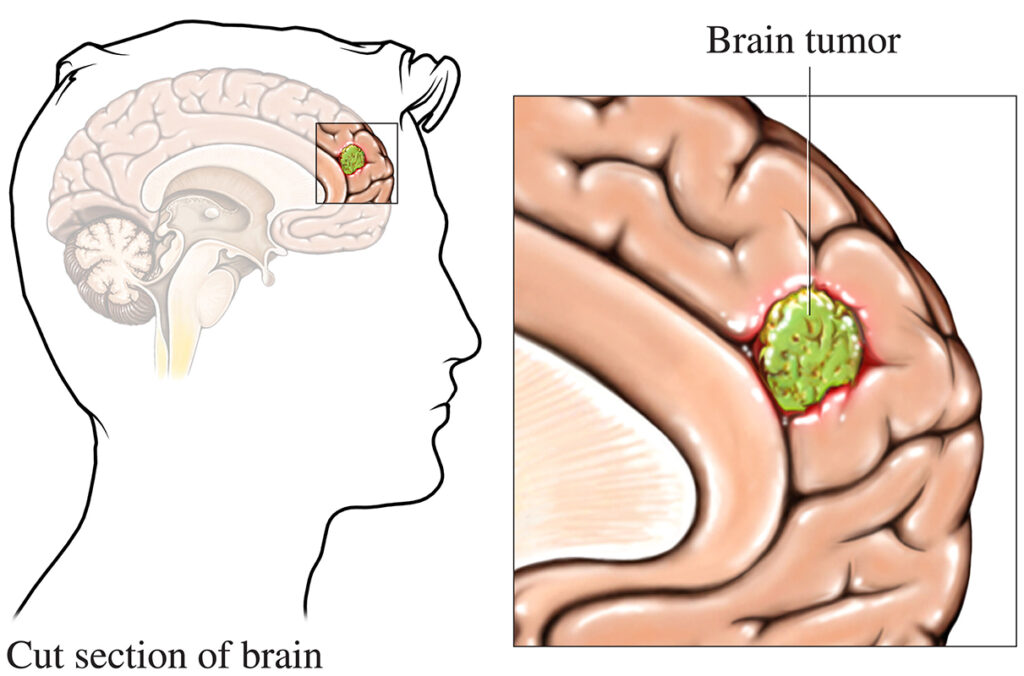
A neoplasm of the brain, also referred to as a brain tumor, is an abnormal growth of cells within the brain or central nervous system (CNS). These tumors can be benign (non-cancerous) or malignant (cancerous) and may arise from brain tissues (primary tumors) or spread from cancers located in other parts of the body (secondary or metastatic tumors). Due to the brain’s complex structure and function, even benign neoplasms can cause significant neurological issues.
Classification of Brain Neoplasms
Primary vs. Secondary Brain Neoplasms
- Primary Brain Neoplasms: Originate from cells within the brain or meninges. These include gliomas, meningiomas, and medulloblastomas.
- Secondary Brain Neoplasms: Metastatic tumors that originate from other organs such as the lungs, breasts, kidneys, or skin.
Benign vs. Malignant Brain Tumors
- Benign: Slow-growing, localized, and generally non-invasive (e.g., meningioma).
- Malignant: Fast-growing, invasive, and capable of spreading (e.g., glioblastoma multiforme).
Major Types of Brain Neoplasms
Gliomas
Gliomas originate from glial cells and constitute the majority of malignant brain tumors.
- Astrocytoma: Arises from astrocytes; ranges from Grade I (pilocytic) to Grade IV (glioblastoma).
- Oligodendroglioma: Originates from oligodendrocytes; tends to grow slower but can become aggressive.
- Ependymoma: Derived from ependymal cells lining the ventricles; occurs in both children and adults.
Meningiomas
Meningiomas arise from the meninges and are typically slow-growing and benign. Despite their benign nature, they can cause significant symptoms due to mass effect and location.
Medulloblastomas
Predominantly found in children, these tumors arise in the cerebellum and are highly malignant, often spreading through cerebrospinal fluid.
Pituitary Adenomas
Develop in the pituitary gland and may secrete excess hormones, leading to endocrine disturbances such as Cushing’s disease or acromegaly.
Schwannomas
These tumors arise from Schwann cells, typically affecting the cranial nerves—especially the vestibular nerve (vestibular schwannoma or acoustic neuroma).
Metastatic Brain Tumors
Common sources include:
- Lung cancer
- Breast cancer
- Melanoma
- Kidney cancer
- Colorectal cancer
Metastases typically localize to the cerebral hemispheres, cerebellum, or brainstem.
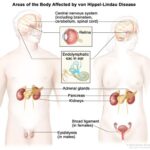
Causes and Risk Factors
- Genetic predispositions: Conditions such as Li-Fraumeni syndrome, Neurofibromatosis type 1 and 2, and Turcot syndrome.
- Radiation exposure: Therapeutic radiation to the head.
- Environmental exposures: Long-term exposure to chemicals like vinyl chloride, formaldehyde.
- Immunosuppression: Increases the risk of CNS lymphomas.
Clinical Presentation of Brain Tumors
Symptoms are largely determined by the tumor’s size, type, and location. Common symptoms include:
- Headaches (often worse in the morning)
- Nausea and vomiting
- Seizures
- Cognitive or personality changes
- Motor weakness or sensory deficits
- Visual disturbances
- Speech or language difficulties
Focal neurological deficits often guide the localization of the tumor.
Diagnostic Methods
Neuroimaging
- Magnetic Resonance Imaging (MRI): Preferred modality for evaluating tumor characteristics.
- Computed Tomography (CT): Useful in emergencies, especially for detecting hemorrhages or calcifications.
Biopsy
Stereotactic or open biopsy provides definitive histopathological diagnosis and molecular profiling, essential for treatment planning.
Functional Imaging
- PET scans: Assess metabolic activity of tumors.
- MR spectroscopy: Identifies biochemical changes in neoplastic tissue.
WHO Tumor Grading System
The World Health Organization (WHO) classifies CNS tumors based on histopathology and molecular markers:
- Grade I: Benign, slow-growing (e.g., pilocytic astrocytoma)
- Grade II: Low-grade malignancy, infiltrative
- Grade III: High-grade malignancy with active mitosis
- Grade IV: Highly aggressive (e.g., glioblastoma multiforme)
Treatment Strategies for Brain Neoplasms
Surgical Resection
The first-line treatment for many brain tumors is maximal safe surgical resection, aiming to remove as much tumor tissue as possible without impairing neurological function.
Radiation Therapy
- External Beam Radiotherapy (EBRT)
- Stereotactic Radiosurgery (SRS): High-precision radiation used for small or inoperable tumors.
Chemotherapy
Common agents include temozolomide, particularly for gliomas. Chemotherapy effectiveness varies based on tumor type and genetic markers like MGMT methylation status.
Targeted Therapy and Immunotherapy
- Bevacizumab (anti-VEGF): Used in recurrent glioblastoma.
- Tumor-treating fields (TTFs): Novel non-invasive approach for glioblastoma.
- Checkpoint inhibitors: Under investigation for brain metastases and gliomas.
Prognosis and Survival Rates
Prognosis depends on several variables:
- Tumor type and grade
- Location
- Age and performance status
- Extent of resection
- Genetic markers
| Tumor Type | 5-Year Survival Rate |
|---|---|
| Pilocytic Astrocytoma | >90% |
| Low-grade Glioma | ~50–60% |
| Glioblastoma Multiforme | ~5% |
| Meningioma (Benign) | >85% |
| Metastatic Brain Tumors | Varies (10–30%) |
Prevention and Monitoring
While most brain tumors are not preventable, genetic counseling and regular surveillance are crucial in high-risk individuals. MRI screening in genetically predisposed patients aids early detection and intervention.
Brain neoplasms represent a complex spectrum of disorders with varying clinical presentations, prognoses, and treatment challenges. Timely diagnosis, multidisciplinary management, and precision medicine approaches have significantly improved outcomes in many patients. Understanding the nuances of each tumor type is vital for delivering optimal care and improving neurological function and quality of life.