Mucormycosis, commonly known as black fungus, is a severe and often fatal fungal infection caused by fungi from the Mucorales order. It primarily affects individuals with compromised immune systems, including those with uncontrolled diabetes, cancer, organ transplants, or COVID-19-related complications. The infection rapidly spreads through tissues, leading to extensive necrosis and requiring urgent medical intervention.

What is Mucormycosis?
Mucormycosis is a rare but aggressive fungal infection caused by molds of the Mucorales family, including Rhizopus, Mucor, and Lichtheimia species. These fungi are ubiquitous in the environment, thriving in soil, decaying organic matter, and even indoor settings. Infection occurs when fungal spores enter the body through inhalation, ingestion, or direct skin wounds.
Types of Mucormycosis
Mucormycosis manifests in different clinical forms, depending on the site of infection:
- Rhino-Orbital-Cerebral Mucormycosis (ROCM) – Affects the sinuses, eyes, and brain, commonly seen in diabetics.
- Pulmonary Mucormycosis – Affects the lungs, often occurring in immunocompromised patients.
- Gastrointestinal Mucormycosis – Rare, but affects the stomach and intestines, seen in malnourished individuals.
- Cutaneous Mucormycosis – Occurs after skin trauma, burns, or surgical wounds.
- Disseminated Mucormycosis – A severe form where the infection spreads through the bloodstream to multiple organs.
Causes and Risk Factors
Mucormycosis occurs primarily in individuals with weakened immune defenses.
Primary Risk Factors
- Uncontrolled Diabetes Mellitus – High blood sugar levels support fungal growth.
- COVID-19 Infection & Steroid Use – Immunosuppressive effects increase susceptibility.
- Organ Transplants & Immunosuppressive Therapy – Reduces immune response against infections.
- Cancer & Chemotherapy – Lowers neutrophil count, allowing fungal invasion.
- Prolonged ICU Stay & Mechanical Ventilation – Increases risk of nosocomial (hospital-acquired) infections.
Symptoms of Mucormycosis
Rhino-Orbital-Cerebral Mucormycosis
- Facial swelling and pain
- Nasal congestion with black discharge
- Vision loss and eye protrusion (proptosis)
- Headache and altered mental status
Pulmonary Mucormycosis
- Fever and chest pain
- Cough with bloody sputum (hemoptysis)
- Shortness of breath (dyspnea)
Gastrointestinal Mucormycosis
- Severe abdominal pain
- Vomiting blood (hematemesis)
- Gastrointestinal perforation leading to sepsis
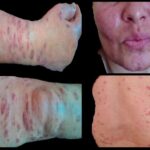
Cutaneous Mucormycosis
- Painful, necrotic skin lesions
- Fungal abscesses and tissue destruction
Disseminated Mucormycosis
- Multi-organ failure
- Severe sepsis and altered consciousness
Diagnosis of Mucormycosis
Early and accurate diagnosis is critical for effective treatment.
Clinical Examination
- Facial swelling, black eschar (necrotic tissue)
- Neurological deficits in cerebral involvement
Laboratory & Imaging Tests
- Direct Microscopy & Fungal Culture: Identifies broad, ribbon-like non-septate hyphae.
- Histopathology: Confirms tissue invasion.
- PCR Testing: Detects fungal DNA.
- CT/MRI Scans: Identify extent of sinus, lung, or brain involvement.
Treatment of Mucormycosis
1. Antifungal Therapy
Liposomal Amphotericin B (IV infusion) is the first-line treatment, followed by posaconazole or isavuconazole for long-term maintenance.
- Amphotericin B: Administered intravenously to halt fungal spread.
- Posaconazole/Isavuconazole: Used as step-down therapy after initial control.
2. Surgical Debridement
- Urgent surgical removal of infected tissues is crucial to prevent fungal spread.
- Endoscopic sinus surgery for rhino-orbital cases.
- Lung resection (lobectomy) for pulmonary involvement.
3. Supportive Care
- Control blood sugar levels in diabetic patients.
- Reduce corticosteroid use when possible.
- Oxygen therapy and ICU management in severe cases.
Prevention Strategies
For High-Risk Individuals
- Strict blood sugar control in diabetics.
- Minimize prolonged corticosteroid and immunosuppressant use.
- Maintain proper hygiene, including wearing masks in dusty environments.
Hospital Infection Control Measures
- Sterile environment in ICUs.
- Regular disinfection of ventilators and oxygen supplies.
- Early detection and isolation of suspected cases.
Prognosis and Mortality Rate
Mucormycosis has a high mortality rate, ranging from 30% to 80%, depending on:
- Site of infection (Cerebral and disseminated forms have worse outcomes).
- Speed of diagnosis and intervention.
- Patient’s underlying health conditions.
Mucormycosis is a rapidly progressive and life-threatening fungal infection requiring early detection, aggressive antifungal therapy, and surgical intervention. High-risk individuals should take preventive measures to reduce their chances of infection. Ongoing research in antifungal drug development and immunotherapy aims to improve patient outcomes.