Mucopolysaccharidosis type II (MPS II), also known as Hunter syndrome, is a rare X-linked lysosomal storage disorder caused by a deficiency in the enzyme iduronate-2-sulfatase (IDS). This enzyme is crucial for the breakdown of glycosaminoglycans (GAGs), specifically dermatan sulfate and heparan sulfate. The accumulation of these substances leads to progressive damage to multiple organs, including the brain, heart, and joints.

What is Mucopolysaccharidosis Type II (MPS II)?
MPS II is one of the mucopolysaccharidosis (MPS) disorders, characterized by the body’s inability to properly degrade glycosaminoglycans. Unlike most other MPS disorders, which follow an autosomal recessive inheritance pattern, MPS II is inherited in an X-linked recessive manner. This means it primarily affects males, while females are typically carriers.
Types of MPS II
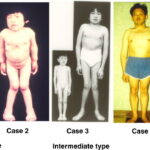
MPS II presents in two primary forms:
| Type | Severity | Symptoms | Life Expectancy |
|---|---|---|---|
| Severe MPS II | Progressive and life-threatening | Cognitive decline, skeletal abnormalities, respiratory complications, cardiac involvement | Often fatal by the teenage years |
| Mild (Attenuated) MPS II | Less severe, slower progression | No cognitive decline, but joint stiffness, heart valve issues, and airway problems persist | Can survive into adulthood |
Causes and Genetic Basis of MPS II
MPS II is caused by mutations in the IDS gene, located on the X chromosome. These mutations lead to a deficiency or complete absence of the iduronate-2-sulfatase enzyme, preventing the proper breakdown of glycosaminoglycans.
Symptoms of MPS II
MPS II symptoms vary in severity depending on whether the individual has the severe or mild form of the disease. Symptoms typically appear between ages 2 and 4 and progressively worsen over time.
Early Signs and Symptoms
- Developmental delays (severe form)
- Frequent ear infections and respiratory issues
- Enlarged liver and spleen (hepatosplenomegaly)
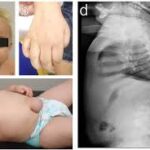
- Coarse facial features (thickened lips, enlarged tongue)
- Delayed growth and short stature
Neurological and Cognitive Symptoms
- Intellectual disability (only in the severe form)
- Hyperactivity and behavioral problems
- Hydrocephalus (fluid accumulation in the brain)
Skeletal and Musculoskeletal Symptoms
- Joint stiffness and contractures
- Dysostosis multiplex (abnormal bone development)
- Short fingers with claw-like hands
Cardiovascular and Respiratory Symptoms
- Heart valve abnormalities
- Obstructive airway disease
- Sleep apnea
Ophthalmological and Hearing Issues
- Hearing loss (conductive or sensorineural)
- Mild corneal clouding (less severe than other MPS types)
Diagnosis of MPS II
Clinical Examination and Medical History
Physicians diagnose MPS II based on:
- Physical signs (coarse facial features, skeletal abnormalities)
- Developmental history and growth patterns
Laboratory and Genetic Tests
- Enzyme Assay: Measures iduronate-2-sulfatase activity in blood or fibroblasts.
- Urinary Glycosaminoglycan (GAG) Analysis: Detects elevated dermatan and heparan sulfate.
- Genetic Testing: Confirms mutations in the IDS gene.
Imaging and Other Tests
- X-rays: Identify skeletal abnormalities.
- Echocardiogram: Evaluates heart valve function.
- MRI/CT Scan: Detects brain and spinal cord complications.
Treatment Options for MPS II
Currently, there is no cure for MPS II, but treatments aim to manage symptoms, slow progression, and improve quality of life.
1. Enzyme Replacement Therapy (ERT)
Idursulfase (Elaprase) is an FDA-approved enzyme replacement therapy for MPS II.
- Administered via intravenous infusion weekly.
- Helps reduce organ enlargement and improve joint mobility.
- Does not significantly cross the blood-brain barrier, limiting its effectiveness for neurological symptoms.
2. Hematopoietic Stem Cell Transplantation (HSCT)
- Rarely recommended due to limited effectiveness in treating neurological symptoms.
- More beneficial for other types of MPS disorders than for MPS II.
3. Supportive and Symptomatic Treatments
- Physical Therapy: Improves joint flexibility and reduces stiffness.
- Surgical Interventions: Helps correct airway obstructions, hernias, and heart abnormalities.
- Hearing Aids: Assist with hearing loss.
- Respiratory Support: Includes CPAP therapy or tracheostomy for severe airway obstruction.
Prognosis and Life Expectancy
The prognosis for MPS II depends on whether the individual has the severe or attenuated form:
- Severe MPS II: Without treatment, life expectancy is usually 10-15 years, though ERT may extend survival.
- Mild MPS II: Life expectancy can reach 50-60 years, with management of symptoms.
Research and Emerging Therapies
Ongoing research aims to develop more effective treatments:
- Gene Therapy: Investigating methods to deliver a functional IDS gene to affected cells.
- Blood-Brain Barrier Penetrant ERT: Studies are testing enzymes capable of crossing the blood-brain barrier to address neurological symptoms.
- Substrate Reduction Therapy (SRT): Aims to reduce glycosaminoglycan production at the source.
Mucopolysaccharidosis type II (Hunter syndrome) is a complex, progressive disorder that primarily affects males. While enzyme replacement therapy and symptomatic treatments can improve quality of life, ongoing research offers hope for more effective solutions. Early diagnosis and intervention are essential to managing the condition and maximizing life expectancy.