Morganella morganii, a gram-negative bacterium, is an often-overlooked pathogen that plays a significant role in urinary tract infections (UTIs). Though it is not as widely recognized as other common UTI-causing bacteria like E. coli, Morganella morganii can be a formidable agent in urinary tract infections, particularly in hospital settings and among individuals with underlying health conditions. This article provides a comprehensive exploration of Morganella morganii urinary tract infections, detailing their causes, symptoms, diagnosis, and treatment options.

What is Morganella Morganii?
Morganella morganii is a facultatively anaerobic bacterium that is typically found in the gastrointestinal tract of humans and animals. It is a part of the family Enterobacteriaceae, which also includes E. coli, Klebsiella, and Proteus species. While generally considered a harmless member of the gut microbiota, it can become pathogenic under certain conditions, leading to infections in various parts of the body, including the urinary tract.
Morganella morganii is known for its ability to produce urease, an enzyme that breaks down urea into ammonia and carbon dioxide. This enzyme can cause an increase in urinary pH, creating a more alkaline environment that supports bacterial growth. This characteristic makes it particularly adept at causing urinary tract infections, especially in individuals who have a history of urinary retention, catheter use, or compromised immune systems.
Causes of Morganella Morganii Urinary Tract Infections
Like other UTI-causing bacteria, Morganella morganii can enter the urinary tract through several means. The most common routes include:
- Ascending Infection: Most UTIs caused by Morganella morganii occur via the ascending route, where bacteria from the perineum travel up the urethra and into the bladder. This route is most common in sexually active women, who are more susceptible to UTIs due to their shorter urethras.
- Catheterization: In healthcare settings, Morganella morganii can infect the urinary tract via urinary catheters. Indwelling catheters can introduce bacteria directly into the bladder, increasing the risk of infection.
- Underlying Health Conditions: Certain conditions, such as diabetes, immunosuppressive therapies, or spinal cord injuries, can create an environment where Morganella morganii is more likely to thrive and cause infection. These conditions can impair the body’s natural defenses against urinary pathogens.
- Urinary Retention: Individuals with conditions like enlarged prostate or neurogenic bladder, which affect the ability to fully empty the bladder, are at a heightened risk for developing UTIs caused by Morganella morganii due to stagnant urine acting as a breeding ground for bacteria.
Symptoms of Morganella Morganii Urinary Tract Infections
UTIs caused by Morganella morganii typically present with the same symptoms as those caused by other bacterial pathogens. The most common symptoms include:
- Dysuria (Painful Urination): A burning sensation during urination is one of the hallmark signs of a UTI caused by Morganella morganii.
- Frequent Urge to Urinate: A persistent need to urinate, often accompanied by the sensation that the bladder is not completely empty, is common in Morganella morganii UTIs.
- Cloudy or Foul-Smelling Urine: Urine may appear cloudy and emit a strong, unpleasant odor due to the production of ammonia by the bacteria’s urease activity.
- Pelvic or Lower Abdominal Pain: Discomfort or pain in the lower abdomen or pelvis can accompany a UTI, especially as the infection progresses.
- Hematuria (Blood in Urine): In some cases, Morganella morganii infections can lead to blood in the urine, which may be visible or detected during urinalysis.
- Fever and Malaise: In more severe cases, especially when the infection ascends to the kidneys, systemic symptoms such as fever, chills, and general malaise may occur.
Diagnosis of Morganella Morganii Urinary Tract Infection
Diagnosing a UTI caused by Morganella morganii involves a series of clinical and laboratory steps:
- Urine Culture: The definitive method for diagnosing any bacterial UTI, including one caused by Morganella morganii, is a urine culture. A sample of urine is cultured in a laboratory to identify the presence of bacterial growth and determine the specific strain of bacteria involved.
- Antibiotic Sensitivity Testing: Once Morganella morganii is identified, it is crucial to perform antibiotic sensitivity testing to determine which antibiotics are most effective in treating the infection. This step is particularly important due to the bacterium’s ability to develop resistance to commonly used antibiotics.
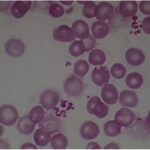
- Urinalysis: A routine urinalysis may reveal the presence of leukocytes, red blood cells, and bacteria in the urine, providing preliminary evidence of a UTI.
- Imaging Studies: In cases where the infection is severe or recurrent, imaging studies such as ultrasound or CT scans may be used to rule out complications like kidney involvement or anatomical abnormalities.
Treatment Options for Morganella Morganii Urinary Tract Infections
Treatment for UTIs caused by Morganella morganii typically involves the use of antibiotics. The choice of antibiotic depends on the results of the urine culture and antibiotic sensitivity testing. Some common treatments for Morganella morganii UTIs include:
- Fluoroquinolones: Drugs such as ciprofloxacin and levofloxacin are commonly used to treat UTIs caused by Morganella morganii, as they are effective against a wide range of gram-negative bacteria.
- Trimethoprim-Sulfamethoxazole (TMP-SMX): This combination antibiotic is often used for uncomplicated UTIs, although resistance rates for Morganella morganii may vary.
- Beta-lactam/Beta-lactamase Inhibitors: In cases of resistance to other antibiotics, medications such as amoxicillin-clavulanate may be considered.
- Carbapenems: For complicated or hospital-acquired infections, carbapenems like meropenem or imipenem may be used, especially when resistance to other antibiotics is present.
In addition to antibiotics, patients may be advised to increase fluid intake to help flush the bacteria from the urinary tract and relieve symptoms. Pain relievers such as acetaminophen or ibuprofen may also be recommended to manage discomfort.
Prevention of Morganella Morganii Urinary Tract Infections
Preventing UTIs caused by Morganella morganii involves several strategies, particularly for individuals at higher risk:
- Proper Hygiene: Regular cleansing of the genital area, especially after urination and sexual activity, can help prevent the spread of bacteria to the urinary tract.
- Hydration: Drinking plenty of fluids, particularly water, helps to flush bacteria from the urinary tract and prevent infections.
- Avoiding Catheter Use: When possible, avoiding the use of urinary catheters can reduce the risk of infection. If catheters are necessary, proper sterile technique should be followed to minimize bacterial introduction.
- Prompt Treatment of UTIs: Early treatment of any urinary tract infection is crucial to prevent the infection from progressing to more severe forms or becoming chronic.
Complications of Morganella Morganii UTIs
While many UTIs caused by Morganella morganii can be effectively treated with antibiotics, untreated or severe infections can lead to complications, including:
- Pyelonephritis: Infection may spread to the kidneys, causing a more serious kidney infection known as pyelonephritis. Symptoms include fever, flank pain, and nausea.
- Urosepsis: In rare cases, a UTI caused by Morganella morganii can progress to sepsis, a life-threatening condition that occurs when the infection spreads throughout the body.
- Chronic UTIs: Recurrent infections can lead to long-term bladder dysfunction and potentially increase the risk of kidney damage.
Morganella morganii urinary tract infections, though less common than other bacterial infections, can be serious and require prompt diagnosis and treatment. Understanding the causes, symptoms, and treatment options for these infections is essential for managing the condition and preventing complications. With the right medical intervention, individuals affected by Morganella morganii UTIs can expect full recovery and a return to good health.