Mismatch repair deficient (MMR-d) endometrial cancer is a subtype of endometrial cancer characterized by defects in the DNA mismatch repair system. This impairment leads to microsatellite instability (MSI) and increases the likelihood of genetic mutations that contribute to cancer progression. MMR deficiency is often associated with Lynch syndrome but can also arise sporadically.
Causes and Risk Factors
Genetic Mutations
The primary cause of MMR deficiency in endometrial cancer is the loss of function in key mismatch repair genes, such as MLH1, MSH2, MSH6, and PMS2. These mutations prevent the proper correction of DNA replication errors, leading to increased genomic instability.
Lynch Syndrome and Hereditary Factors
Lynch syndrome, an inherited disorder, is one of the most significant risk factors for MMR-d endometrial cancer. Individuals with Lynch syndrome have a higher risk of developing colorectal and endometrial cancers due to germline mutations in MMR genes.
Epigenetic Changes and Sporadic Cases
In some cases, MMR deficiency arises from epigenetic silencing, particularly hypermethylation of the MLH1 promoter, leading to loss of gene function without direct mutations.
Other Contributing Factors
- Obesity: Increased estrogen levels can contribute to endometrial hyperplasia, a precursor to cancer.
- Age: Postmenopausal women are at higher risk.
- Hormonal Therapy: Prolonged estrogen exposure without progesterone balance increases risk.
Diagnosis of MMR-d Endometrial Cancer
Clinical Presentation
Common symptoms include:
- Abnormal vaginal bleeding
- Pelvic pain
- Postmenopausal spotting
- Unexplained weight loss
Diagnostic Techniques
- Histopathological Examination
- Endometrial biopsy to confirm malignancy.
- Immunohistochemistry (IHC) Testing
- Detects loss of MMR protein expression, guiding further genetic testing.
- Microsatellite Instability (MSI) Testing
- High MSI status suggests MMR deficiency.
- Genetic Testing for Lynch Syndrome
- Recommended for patients with strong family history or confirmed MMR deficiency.
Treatment Options
Surgical Management
- Hysterectomy with Bilateral Salpingo-Oophorectomy (BSO)
- The standard treatment for localized disease.
- Lymph Node Dissection
- Assesses the spread and guides further treatment.
Adjuvant Therapy
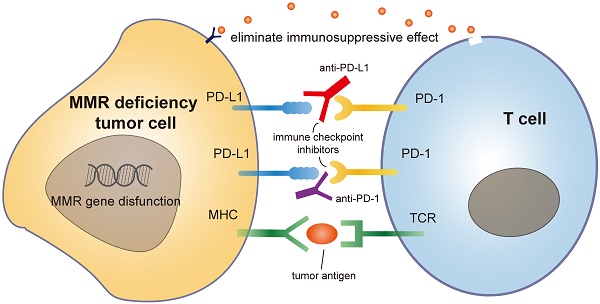
- Immunotherapy
- Pembrolizumab and Dostarlimab, PD-1 inhibitors, are effective in advanced MMR-d endometrial cancer.
- Radiation Therapy
- Used post-surgery for patients at risk of recurrence.
- Chemotherapy
- Carboplatin and Paclitaxel are commonly used for metastatic cases.
Targeted Therapy and Emerging Treatments
- Research is exploring novel checkpoint inhibitors and combination therapies for better outcomes.
Prognosis and Prevention
Survival Rates
Patients with MMR-d endometrial cancer generally have a better response to immunotherapy, improving survival in advanced cases.
Preventative Measures
- Regular Screening for Lynch Syndrome
- Lifestyle Modifications (Healthy diet, weight management, physical activity)
- Early Detection Strategies (Routine gynecologic exams and genetic counseling)
Mismatch repair deficient endometrial cancer presents unique diagnostic and therapeutic challenges. Advances in genetic testing and immunotherapy have significantly improved patient outcomes. Early detection through screening programs and personalized treatment plans remain crucial for managing this subtype effectively.

