Methicillin-resistant Staphylococcus aureus (MRSA) nasal colonization refers to the presence of MRSA bacteria in the nasal passages without causing active infection. While colonization itself does not result in symptoms, it serves as a significant reservoir for potential infections and transmission to others. MRSA is a major public health concern due to its resistance to multiple antibiotics, making infections difficult to treat. This article explores the causes, risk factors, transmission, prevention, and treatment options for MRSA nasal colonization.
Understanding MRSA Nasal Colonization
MRSA is a type of Staphylococcus aureus that has developed resistance to methicillin and other beta-lactam antibiotics. Nasal colonization means that MRSA is present in the nasal passages but does not cause immediate harm. However, colonized individuals can unknowingly spread the bacteria to others or develop infections if their immune system becomes compromised.
Risk Factors for MRSA Nasal Colonization
Several factors contribute to MRSA nasal colonization, including:
- Healthcare Exposure: Patients who have been hospitalized or undergone medical procedures are at higher risk.
- Antibiotic Use: Frequent or inappropriate antibiotic use can lead to resistance and colonization.
- Weakened Immune System: Individuals with chronic illnesses, immunodeficiencies, or undergoing chemotherapy are more susceptible.
- Close Contact Environments: MRSA spreads easily in crowded settings such as nursing homes, prisons, and athletic facilities.
- Poor Hygiene Practices: Inadequate handwashing and sharing personal items increase the risk of colonization.
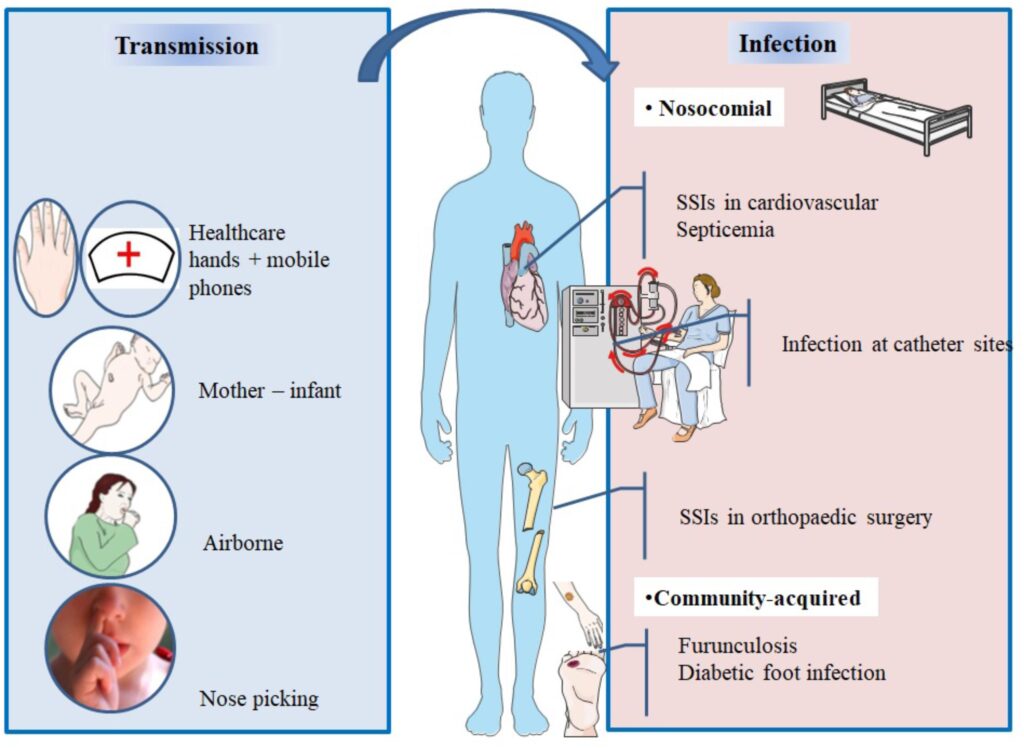
Transmission of MRSA
MRSA spreads through direct contact with contaminated surfaces, skin-to-skin interactions, or respiratory droplets. Healthcare workers and family members of colonized individuals are at a higher risk of acquiring and transmitting the bacteria. MRSA can also enter the body through cuts, abrasions, or medical devices such as catheters, leading to serious infections.
Complications of MRSA Colonization
While colonization alone does not cause disease, it increases the risk of infections such as:
- Skin and Soft Tissue Infections: Abscesses, cellulitis, and wound infections.
- Pneumonia: MRSA-related lung infections can be severe, especially in hospitalized patients.
- Bloodstream Infections: Bacteremia and sepsis can occur if MRSA enters the bloodstream.
- Surgical Site Infections: Postoperative MRSA infections prolong recovery and may lead to complications.
MRSA Nasal Decolonization Strategies
To reduce MRSA carriage and prevent infections, nasal decolonization methods include:
- Topical Antibiotics: Mupirocin ointment applied to the nasal passages effectively eradicates MRSA.
- Antiseptic Body Washes: Chlorhexidine or povidone-iodine washes lower bacterial load on the skin.
- Oral Antibiotics: Reserved for high-risk patients under medical supervision.
- Improved Hygiene: Regular handwashing and avoiding shared personal items prevent reinfection.
- Environmental Cleaning: Frequent disinfection of surfaces reduces contamination risks.
Preventing MRSA Transmission
- Hand Hygiene: Proper handwashing with soap and alcohol-based sanitizers minimizes bacterial spread.
- Contact Precautions: Healthcare facilities should implement isolation measures for MRSA-positive patients.
- Personal Protective Equipment (PPE): Use of gloves and masks when caring for colonized individuals.
- Surveillance Programs: Regular screening of high-risk patients in hospitals aids early detection and containment.
MRSA nasal colonization is a significant public health concern, serving as a hidden reservoir for potential infections and transmission. Understanding risk factors, transmission pathways, and effective decolonization methods is crucial for reducing MRSA-related complications. Proper hygiene, medical interventions, and stringent infection control measures are essential in preventing MRSA spread and ensuring better health outcomes.