Methemoglobinemia is a rare but potentially serious blood disorder where methemoglobin levels in the blood rise abnormally, impairing oxygen delivery to tissues. This condition can be congenital or acquired and requires timely diagnosis and treatment to prevent severe complications.
What is Methemoglobinemia?
Methemoglobinemia occurs when hemoglobin, the protein responsible for carrying oxygen in the blood, is converted into methemoglobin. Unlike normal hemoglobin, methemoglobin cannot effectively release oxygen to body tissues, leading to hypoxia.
Types of Methemoglobinemia
- Congenital Methemoglobinemia – A genetic condition caused by mutations in the CYB5R gene, leading to a deficiency in cytochrome b5 reductase, an enzyme responsible for converting methemoglobin back to hemoglobin.
- Acquired Methemoglobinemia – Caused by exposure to certain chemicals, medications, or environmental toxins, such as nitrates, benzocaine, and aniline dyes.
Causes and Risk Factors
Congenital Causes
- Cytochrome b5 reductase deficiency
- Hemoglobin M disease (a structural abnormality in hemoglobin)
Acquired Causes
- Chemical and Drug Exposure: Nitrate-contaminated water, benzocaine, dapsone, nitrites, sulfonamides
- Industrial and Environmental Toxins: Aniline dyes, fertilizers, certain herbicides, and cigarette smoke
- Food Sources: Excessive consumption of nitrate-rich foods, such as leafy greens and cured meats
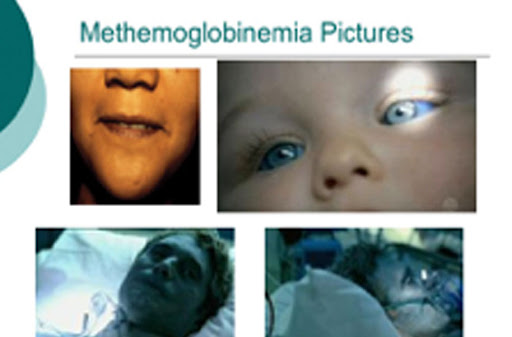
Symptoms of Methemoglobinemia
Symptoms depend on the level of methemoglobin in the blood and may include:
- Cyanosis (bluish skin, lips, and nail beds)
- Shortness of breath
- Fatigue and weakness
- Headaches
- Dizziness
- Confusion
- Seizures (in severe cases)
- Coma (in extreme cases)
Diagnosis
Clinical Examination
- Observing cyanosis that does not improve with oxygen therapy
Laboratory Tests
- Arterial Blood Gas (ABG) Analysis: Identifies oxygen saturation levels
- Methemoglobin Level Test: Measures the percentage of methemoglobin in the blood
- Pulse Oximetry: May show falsely low oxygen saturation
- Genetic Testing: Determines hereditary methemoglobinemia
Treatment Options
Mild Cases
- Often resolve without medical intervention if exposure to the causative agent is discontinued
Severe Cases
- Methylene Blue Injection: Acts as an electron donor to convert methemoglobin back to hemoglobin
- Ascorbic Acid (Vitamin C): Reduces methemoglobin levels in mild cases
- Oxygen Therapy: Administered to improve oxygenation
- Exchange Transfusion: In extreme cases where other treatments fail
Prevention Strategies
- Avoidance of High-Nitrate Foods and Water: Testing well water for nitrate contamination
- Proper Medication Use: Avoiding excessive use of benzocaine-containing products
- Monitoring in High-Risk Individuals: Newborns and individuals with genetic predisposition should be carefully monitored
Prognosis
With timely diagnosis and appropriate treatment, the prognosis for methemoglobinemia is generally favorable. Congenital cases require lifelong management, while acquired cases improve with the removal of the causative agent and medical intervention.
Methemoglobinemia is a serious condition that can significantly impact oxygen transport in the blood. Understanding its causes, symptoms, and treatment options is essential for effective management and prevention. Early diagnosis and timely medical intervention can lead to successful recovery and prevent complications.

