Metastatic non-small cell lung cancer (NSCLC) with epidermal growth factor receptor (EGFR) exon 19 deletion is a distinct subtype of lung cancer characterized by genetic mutations that drive tumor growth. Understanding its molecular profile is crucial for optimizing treatment strategies, improving prognosis, and enhancing patient outcomes.
Understanding EGFR Exon 19 Deletion in NSCLC
EGFR mutations are among the most common alterations found in NSCLC, particularly in adenocarcinoma. Exon 19 deletion accounts for approximately 45-50% of EGFR-mutated NSCLC cases, making it a critical biomarker for targeted therapy selection. The mutation leads to constitutive activation of the EGFR pathway, driving uncontrolled cell proliferation and tumor growth.
Mechanism of Action
EGFR exon 19 deletion removes part of the tyrosine kinase domain, enhancing its activity and increasing tumor aggressiveness. This molecular alteration renders tumors highly sensitive to EGFR tyrosine kinase inhibitors (TKIs), a cornerstone in targeted treatment.
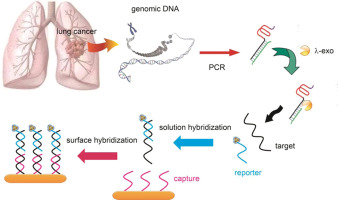
Diagnosis and Testing
Accurate diagnostic testing is essential for identifying EGFR exon 19 deletion in NSCLC. Several methods are utilized:
- Polymerase Chain Reaction (PCR): High sensitivity for detecting EGFR mutations.
- Next-Generation Sequencing (NGS): Comprehensive analysis of multiple gene mutations.
- Fluorescence In Situ Hybridization (FISH): Detects chromosomal alterations.
- Liquid Biopsy: Non-invasive approach using circulating tumor DNA (ctDNA) to monitor mutation status.
Treatment Strategies
First-Line Therapy: EGFR-TKIs
EGFR-TKIs are the gold standard for treating metastatic NSCLC with exon 19 deletion. Key inhibitors include:
- Osimertinib – Third-generation EGFR-TKI, effective against both primary and T790M resistance mutations.
- Erlotinib & Gefitinib – First-generation EGFR-TKIs offering significant response rates.
- Afatinib & Dacomitinib – Second-generation inhibitors with irreversible binding to EGFR.
Combination Therapies
- EGFR-TKIs + Chemotherapy: Studies show adding pemetrexed-based chemotherapy improves survival rates.
- EGFR-TKIs + Anti-angiogenic Therapy: Bevacizumab (VEGF inhibitor) enhances TKI efficacy.
- Immunotherapy Considerations: While checkpoint inhibitors (PD-1/PD-L1) are standard in NSCLC, their role in EGFR-mutant cancers remains limited due to lower response rates.
Resistance Mechanisms and Management
Over time, acquired resistance to EGFR-TKIs develops. Common mechanisms include:
- T790M Mutation (50-60% of cases): Sensitivity to osimertinib.
- MET Amplification: Requires combination therapy targeting MET.
- Small Cell Lung Cancer Transformation: Rare but aggressive progression.
Strategies to overcome resistance:
- Next-generation TKIs (e.g., osimertinib for T790M-positive cases).
- Combination approaches integrating chemotherapy, MET inhibitors, or immunotherapy.
Prognosis and Survival Outcomes
Patients with metastatic NSCLC EGFR exon 19 deletion generally have a more favorable prognosis compared to other NSCLC subtypes when treated with targeted therapy. Median progression-free survival (PFS) with first-line EGFR-TKIs ranges from 10 to 19 months, with overall survival (OS) extending beyond 3 years in some cases.
Emerging Research and Future Directions
- Fourth-Generation EGFR Inhibitors: Designed to overcome resistance mutations.
- Bispecific Antibodies: Targeting both EGFR and MET to enhance response.
- Liquid Biopsy Advancements: Improving real-time monitoring of tumor evolution.
- AI-Driven Drug Discovery: Identifying novel therapeutic targets in EGFR-mutant NSCLC.
Metastatic NSCLC with EGFR exon 19 deletion represents a well-defined molecular subtype with effective targeted treatments available. EGFR-TKIs have revolutionized management, yet challenges such as drug resistance persist. Ongoing research into combination therapies, next-generation inhibitors, and novel biomarkers will further enhance patient outcomes.