Metastatic HER2-positive carcinoma of the breast is an advanced stage of breast cancer in which cancer cells overexpress the human epidermal growth factor receptor 2 (HER2) and spread beyond the breast to distant organs. HER2 amplification drives aggressive tumor growth, making targeted treatment strategies essential for improving patient outcomes.
Understanding HER2-Positive Breast Cancer
HER2-positive breast cancer accounts for approximately 15-20% of all breast cancer cases. It is characterized by excessive HER2 protein production, which leads to rapid cancer cell proliferation. Early detection and targeted therapy have significantly improved survival rates for patients with this subtype.
Pathophysiology of HER2-Positive Breast Cancer
HER2, a tyrosine kinase receptor, belongs to the epidermal growth factor receptor (EGFR) family. When overexpressed, HER2 activates intracellular pathways such as the PI3K/AKT and MAPK pathways, leading to uncontrolled cellular proliferation, angiogenesis, and metastasis.
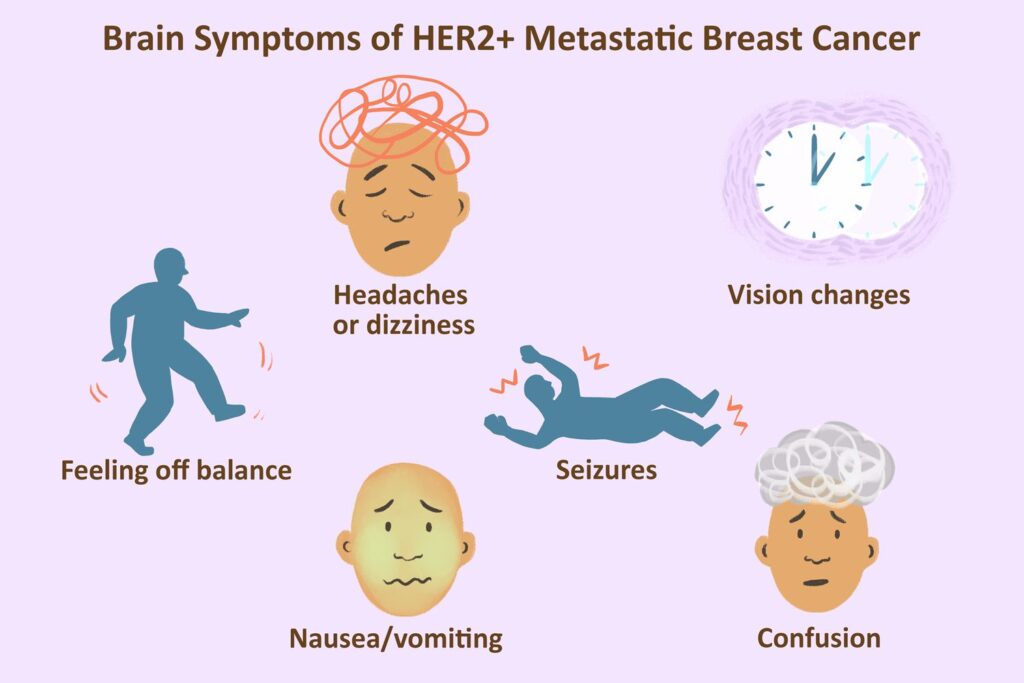
Symptoms of Metastatic HER2-Positive Breast Cancer
Metastatic breast cancer can present with diverse symptoms depending on the site of metastasis:
- Bone metastases: Bone pain, fractures, hypercalcemia.
- Lung metastases: Chronic cough, breathlessness, pleural effusion.
- Liver metastases: Jaundice, abdominal pain, elevated liver enzymes.
- Brain metastases: Headaches, seizures, neurological deficits.
Diagnosis and Staging
Diagnostic Tests:
- Immunohistochemistry (IHC): Assesses HER2 protein expression.
- Fluorescence In Situ Hybridization (FISH): Detects HER2 gene amplification.
- CT Scan & PET Scan: Identify distant metastases.
- MRI: Used to evaluate brain metastases.
- Biopsy: Confirms the presence of HER2 overexpression.
Staging System (TNM Classification):
- T (Tumor): Size and extent of the primary tumor.
- N (Nodes): Lymph node involvement.
- M (Metastasis): Presence of distant metastases (Stage IV).
Treatment Options for Metastatic HER2-Positive Breast Cancer
1. Targeted Therapy
HER2-directed therapies have revolutionized the treatment landscape:
- Trastuzumab (Herceptin): A monoclonal antibody that blocks HER2 receptors.
- Pertuzumab (Perjeta): Prevents HER2 dimerization, used with trastuzumab.
- Ado-trastuzumab emtansine (T-DM1): Antibody-drug conjugate delivering cytotoxic agents to HER2-positive cells.
- Fam-trastuzumab deruxtecan (Enhertu): A next-generation ADC with a potent chemotherapy payload.
2. Chemotherapy
- Taxanes (Paclitaxel, Docetaxel): Often combined with HER2-targeted therapy.
- Capecitabine: An oral chemotherapy option for patients with progression after trastuzumab.
3. Hormonal Therapy
For patients with hormone receptor (HR)-positive and HER2-positive tumors, hormonal therapy (e.g., Tamoxifen, Aromatase Inhibitors) may be used alongside targeted treatments.
4. Immunotherapy
Immune checkpoint inhibitors, such as Atezolizumab, show potential when combined with chemotherapy in HER2-positive triple-negative breast cancer cases.
5. Radiation Therapy
- Used for palliation in bone, brain, and lung metastases.
- Stereotactic radiosurgery (SRS) is effective for brain lesions.
Emerging Treatments & Clinical Trials
1. Novel HER2 Inhibitors
- Tucatinib (Tukysa): A selective HER2 inhibitor with promising results in brain metastases.
- Neratinib: An irreversible HER2/EGFR inhibitor used in treatment-resistant cases.
2. Bispecific Antibodies
- Zanidatamab: Targets two different HER2 epitopes simultaneously for enhanced efficacy.
3. HER2-Directed CAR-T Therapy
- Ongoing research explores Chimeric Antigen Receptor (CAR)-T cells engineered to target HER2-positive cancer cells.
Prognosis and Survival Rates
- The 5-year survival rate for metastatic HER2-positive breast cancer has improved significantly with targeted therapy.
- Median overall survival (OS): Ranges from 3 to 5 years, depending on treatment response and tumor burden.
- Factors influencing prognosis: Tumor burden, treatment resistance, performance status, and brain metastases.
Supportive Care and Quality of Life
- Pain Management: Opioids, bisphosphonates for bone metastases.
- Nutritional Support: High-protein diet, supplements for cachexia prevention.
- Psychosocial Support: Counseling, patient support groups, mental health care.
Metastatic HER2-positive carcinoma of the breast remains a challenging disease, but advancements in targeted therapy, immunotherapy, and precision medicine have significantly extended survival and improved the quality of life for patients. Continuous research and participation in clinical trials offer hope for better treatment outcomes in the future.