Meningococcal meningitis is a severe bacterial infection that affects the meninges, the protective membranes surrounding the brain and spinal cord. Caused by Neisseria meningitidis, this condition can lead to life-threatening complications, including septicemia, brain damage, and death if left untreated. Early recognition and prompt medical intervention are crucial in managing the disease effectively.
Causes and Risk Factors
Neisseria meningitidis: The Causative Agent
Neisseria meningitidis is a gram-negative diplococcus bacterium that colonizes the nasopharynx in healthy individuals but can invade the bloodstream and central nervous system under certain conditions. There are 13 known serogroups, with A, B, C, W, X, and Y being the most common causes of meningococcal meningitis.
Risk Factors
- Age: Infants, young children, and adolescents are at higher risk.
- Crowded Environments: Schools, dormitories, and military barracks facilitate the spread.
- Weakened Immune System: Immunodeficiency conditions increase susceptibility.
- Travel to Endemic Regions: Sub-Saharan Africa’s “meningitis belt” has frequent outbreaks.
- Close Contact: Kissing, coughing, or sharing utensils can transmit bacteria.
Symptoms of Meningococcal Meningitis
Early Symptoms
- Fever and chills
- Severe headache
- Nausea and vomiting
- Sensitivity to light (photophobia)
- Stiff neck
Advanced Symptoms
- Altered mental status (confusion, delirium, coma)
- Seizures
- Rapid breathing
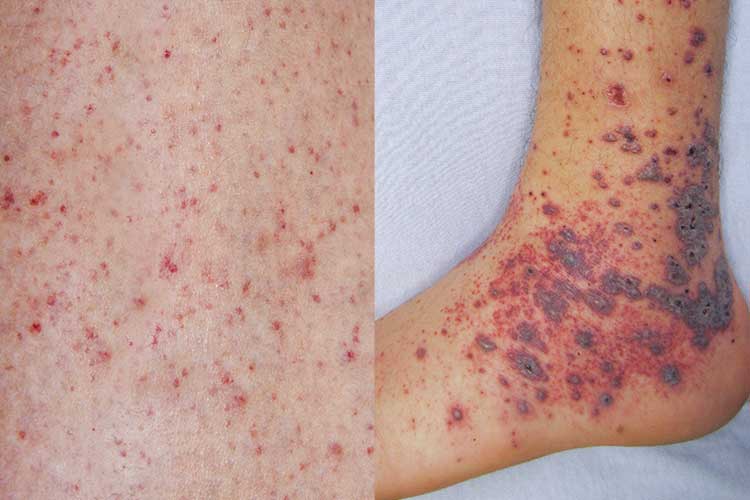
- Purpuric rash (a hallmark of meningococcemia)
- Shock and multi-organ failure in severe cases
Diagnosis
Laboratory Tests
- Cerebrospinal Fluid (CSF) Analysis: Lumbar puncture to detect bacterial presence.
- Blood Cultures: Identification of N. meningitidis in the bloodstream.
- Polymerase Chain Reaction (PCR): Rapid detection of bacterial DNA.
- Gram Stain: Microscopic examination of CSF samples.
Treatment Options
Antibiotic Therapy
Immediate antibiotic administration is critical to reducing mortality. Recommended antibiotics include:
- Ceftriaxone or Cefotaxime: First-line treatment.
- Penicillin G: Alternative in susceptible strains.
- Rifampin or Ciprofloxacin: Prophylaxis for close contacts.
Supportive Care
- Intravenous fluids for hydration
- Oxygen therapy for respiratory distress
- Anticonvulsants for seizure management
- Intensive care for severe cases
Prevention and Vaccination
Meningococcal Vaccines
Vaccination is the most effective way to prevent meningococcal meningitis. Available vaccines include:
- MenACWY Vaccine: Protects against serogroups A, C, W, and Y.
- MenB Vaccine: Specifically targets serogroup B.
- Routine Vaccination Schedule:
- Adolescents at 11–12 years, with a booster at 16 years
- High-risk individuals, such as those with complement deficiencies
Preventive Measures
- Practicing good hygiene (frequent handwashing, avoiding close contact with infected individuals)
- Early identification and treatment of carriers
- Chemoprophylaxis for exposed individuals
Complications of Meningococcal Meningitis
Even with prompt treatment, complications can arise, including:
- Hearing Loss: Damage to auditory nerves
- Neurological Deficits: Cognitive impairment, seizures
- Limb Amputation: Resulting from meningococcemia
- Septic Shock: Can lead to organ failure and death
Meningococcal meningitis is a medical emergency requiring rapid diagnosis and treatment. Vaccination remains the best preventive measure, significantly reducing the incidence of outbreaks. Awareness, early intervention, and improved healthcare strategies are essential in mitigating the impact of this potentially fatal disease.

