Bacterial mastitis is a significant health concern that primarily affects lactating women but can also occur in non-lactating individuals. Understanding this condition is crucial for timely intervention and effective management. This guide delves into the causes, symptoms, treatment, and prevention strategies for bacterial mastitis.
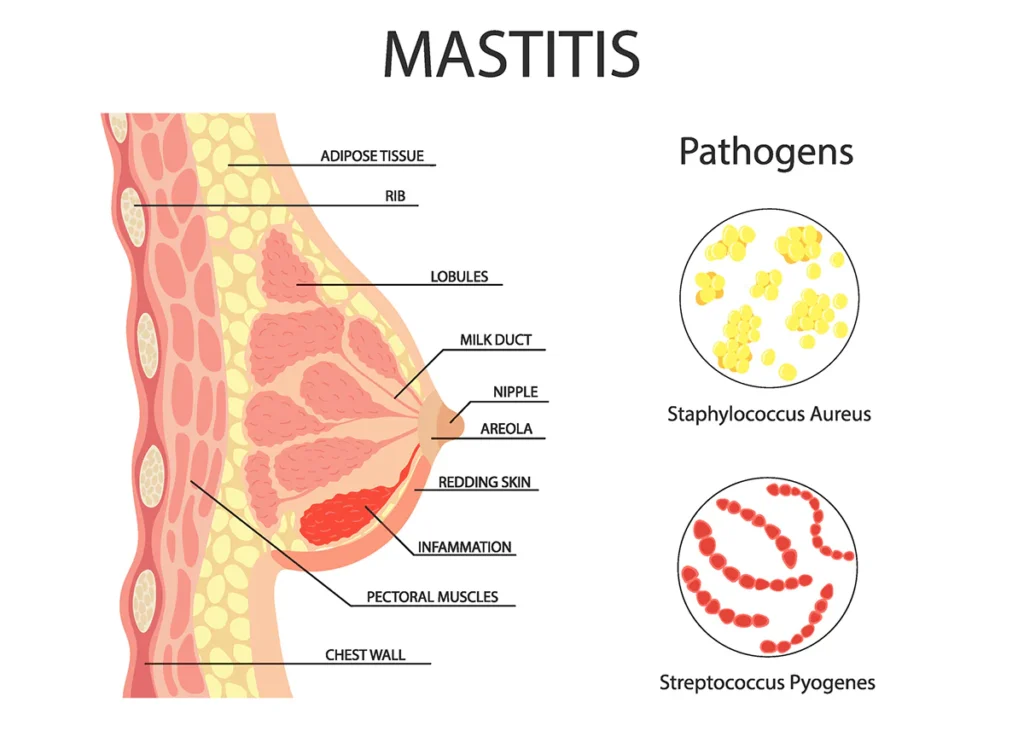
Its an inflammation of the breast tissue caused by a bacterial infection. It often occurs during breastfeeding when bacteria, typically Staphylococcus aureus or Streptococcus species, enter the breast through cracked or sore nipples. The infection leads to localized pain, swelling, and other systemic symptoms.
Common Causes of Bacterial Mastitis
The primary factors contributing to bacterial mastitis include:
- Milk Stasis:
- Incomplete emptying of the breast can lead to milk accumulation, creating an environment conducive to bacterial growth.
- Nipple Trauma:
- Cracks or sores on the nipple surface provide entry points for bacteria.
- Blocked Milk Ducts:
- Obstructions in milk flow can result in localized inflammation and bacterial proliferation.
- Weakened Immunity:
- Stress, fatigue, or underlying health issues can compromise the immune system, increasing susceptibility.
- Poor Hygiene Practices:
- Insufficient breast hygiene during breastfeeding can introduce bacteria.
Symptoms of Bacterial Mastitis
Bacterial mastitis presents with a range of symptoms, including:
- Localized breast pain and tenderness
- Redness and warmth over the affected area
- Swelling and firmness of the breast tissue
- Flu-like symptoms, such as fever and chills
- Fatigue and malaise
- A burning sensation during breastfeeding
Severe cases may lead to abscess formation, requiring immediate medical intervention.
Diagnosis
A healthcare provider will typically diagnose bacterial mastitis based on clinical symptoms and physical examination. In cases of recurrent or severe infections, additional tests may include:
- Breast Milk Culture:
- Identifies the causative bacteria and guides antibiotic therapy.
- Ultrasound Imaging:
- Detects abscesses or blocked ducts.
Treatment of Bacterial Mastitis
Timely and appropriate treatment is essential to prevent complications. Common treatment modalities include:
1. Antibiotics
- Prescribed to target the specific bacterial strain identified through culture.
- Common choices: Dicloxacillin, Cephalexin, or Clindamycin.
2. Breastfeeding Management
- Continue breastfeeding or pumping to maintain milk flow and prevent milk stasis.
- Employ proper latching techniques to minimize nipple trauma.
3. Pain Management
- Over-the-counter analgesics like ibuprofen or acetaminophen to alleviate pain and inflammation.
4. Supportive Measures
- Warm compresses to relieve discomfort.
- Adequate hydration and rest to support the immune response.
Prevention Strategies
Preventing bacterial mastitis involves adopting proactive measures:
- Effective Breastfeeding Techniques:
- Ensure proper latch to minimize nipple trauma.
- Frequent Feeding or Pumping:
- Prevent milk stasis by emptying the breasts regularly.
- Nipple Care:
- Keep nipples clean and moisturized to prevent cracks.
- Good Hygiene Practices:
- Wash hands before breastfeeding or handling the breasts.
- Prompt Attention to Symptoms:
- Address early signs of infection to prevent progression.
When to Seek Medical Attention - Seek medical care if:
- Symptoms persist despite home remedies.
- There is no improvement within 24-48 hours of starting antibiotics.
- An abscess develops, characterized by severe pain, a lump, or pus discharge.
MYHEALTHMAG
- Address early signs of infection to prevent progression.