Meningitis is an inflammatory condition affecting the meninges, the protective membranes surrounding the brain and spinal cord. While viral and bacterial infections are common causes, meningitis due to Bacteroides species is relatively rare but serious. Bacteroides are anaerobic bacteria commonly found in the human gut, but they can cause severe infections when they enter the bloodstream or central nervous system (CNS). This article provides a comprehensive overview of the causes, symptoms, diagnosis, and treatment of Bacteroides meningitis.
Causes and Risk Factors
Meningitis due to Bacteroides is often associated with infections in other parts of the body, such as:
- Sinus infections
- Otitis media (middle ear infection)
- Dental infections
- Head trauma or neurosurgical procedures
- Brain abscesses
- Sepsis leading to hematogenous spread
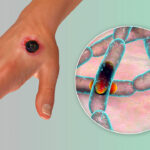
Among the Bacteroides species, Bacteroides fragilis is the most commonly implicated in CNS infections due to its ability to resist host immune defenses and produce virulence factors.
Symptoms of Bacteroides Meningitis
Patients with Bacteroides meningitis may exhibit classic signs of bacterial meningitis, including:
- Severe headache
- Neck stiffness (nuchal rigidity)
- Fever and chills
- Nausea and vomiting
- Altered mental status (confusion, disorientation, or coma)
- Seizures
- Photophobia (sensitivity to light)
Given the aggressive nature of this infection, early detection is crucial to prevent complications such as brain abscesses, hydrocephalus, or neurological deficits.
Diagnosis and Laboratory Testing
Diagnosing Bacteroides meningitis requires a combination of clinical evaluation and laboratory investigations:
1. Cerebrospinal Fluid (CSF) Analysis
A lumbar puncture is performed to collect CSF, which may show:
- Elevated white blood cell count (pleocytosis)
- Increased protein levels
- Decreased glucose concentration
- Gram stain and anaerobic cultures revealing Bacteroides species
2. Blood Cultures
Since Bacteroides infections often stem from systemic spread, blood cultures may confirm the presence of bacteremia.
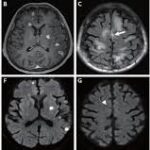
3. Imaging Studies
- CT scan or MRI of the brain to detect abscesses, hydrocephalus, or signs of increased intracranial pressure.
Treatment Strategies
1. Antibiotic Therapy
Immediate antibiotic treatment is essential. Since Bacteroides species are resistant to many conventional antibiotics, the following options are typically used:
- Metronidazole (first-line therapy for anaerobic infections)
- Carbapenems (e.g., meropenem, imipenem)
- Beta-lactam/beta-lactamase inhibitor combinations (e.g., piperacillin-tazobactam)
- Clindamycin (alternative in some cases)
2. Supportive Care
- Intravenous fluids to maintain hydration and electrolyte balance
- Pain management with analgesics
- Seizure control with antiepileptic medications if necessary
- Oxygen therapy for respiratory support if needed
3. Surgical Intervention
In cases involving brain abscesses, surgical drainage may be required to remove infected material and relieve pressure on the brain.
Complications and Prognosis
Without prompt treatment, Bacteroides meningitis can lead to severe complications, including:
- Brain abscesses
- Hydrocephalus
- Persistent neurological deficits (e.g., hearing loss, cognitive impairment)
- Septicemia
- Death
Early and aggressive treatment significantly improves outcomes, but mortality rates remain high in untreated or severe cases.
Prevention and Risk Reduction
Preventive measures include:
- Prompt treatment of head and neck infections
- Proper aseptic techniques during neurosurgical procedures
- Early management of systemic infections to prevent hematogenous spread
Meningitis due to Bacteroides is a rare but life-threatening condition that requires urgent medical attention. Early diagnosis, appropriate antibiotic therapy, and supportive care are essential to improving patient outcomes. Awareness among healthcare professionals about its presentation and management is crucial for timely intervention and reducing morbidity and mortality.