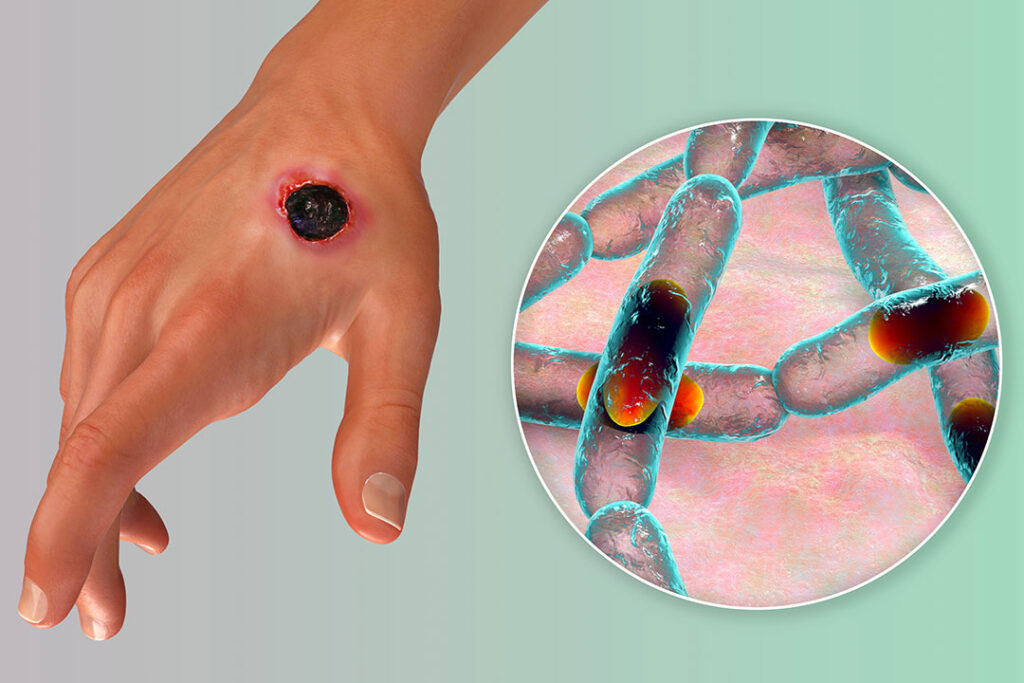
Meningitis due to anthrax is a rare but severe form of bacterial meningitis caused by Bacillus anthracis, the bacterium responsible for anthrax. It primarily affects individuals exposed to anthrax spores through inhalation, ingestion, or cutaneous infection that spreads systemically. This condition has a high mortality rate and requires urgent medical intervention.
Causes and Pathogenesis of Anthrax Meningitis
Anthrax meningitis occurs when Bacillus anthracis enters the bloodstream and crosses the blood-brain barrier, leading to severe inflammation of the meninges. The primary modes of infection include:
- Inhalational Anthrax: The most common precursor to anthrax meningitis, where spores are inhaled and cause systemic infection.
- Cutaneous Anthrax: In rare cases, untreated skin infections can disseminate and lead to meningeal involvement.
- Gastrointestinal Anthrax: Consumption of contaminated meat can result in systemic spread.
Symptoms of Anthrax Meningitis
The symptoms of anthrax meningitis develop rapidly and include:
- Severe headaches
- High fever and chills
- Stiff neck
- Altered mental status (confusion, delirium, or coma)
- Seizures
- Nausea and vomiting
- Photophobia (light sensitivity)
- Coma and death if untreated
Diagnosis of Anthrax Meningitis
Early diagnosis is critical for improving survival rates. Common diagnostic methods include:
- Lumbar Puncture (CSF Analysis): Reveals hemorrhagic cerebrospinal fluid with high protein and low glucose levels.
- Blood Cultures: Detects Bacillus anthracis in systemic circulation.
- Polymerase Chain Reaction (PCR): Identifies bacterial DNA in cerebrospinal fluid or blood.
- CT Scan/MRI: May show brain swelling and hemorrhagic changes.
Treatment of Anthrax Meningitis
Prompt and aggressive treatment is necessary. The main treatment modalities include:
1. Intravenous Antibiotics
- Ciprofloxacin or Doxycycline in combination with Meropenem and Linezolid
- Duration: At least 60 days to prevent relapse
2. Supportive Care
- Ventilation support for respiratory distress
- Fluid management to maintain blood pressure
- Seizure control using anticonvulsants
3. Antitoxins
- Raxibacumab or Obiltoxaximab (monoclonal antibodies) to neutralize anthrax toxins
Prognosis and Survival Rates
Anthrax meningitis has a high mortality rate (over 90%) despite treatment. Early antibiotic administration and intensive care significantly improve survival odds.
Prevention Strategies
- Anthrax Vaccination for high-risk individuals (military personnel, veterinarians, lab workers)
- Avoidance of Contaminated Animal Products
- Post-Exposure Prophylaxis (PEP): 60-day antibiotic regimen following suspected exposure
Meningitis due to anthrax is a rare but highly fatal condition that requires immediate medical intervention. Awareness, rapid diagnosis, and aggressive treatment are essential to improving survival rates. Preventative measures, including vaccination and exposure control, play a crucial role in reducing cases worldwide.