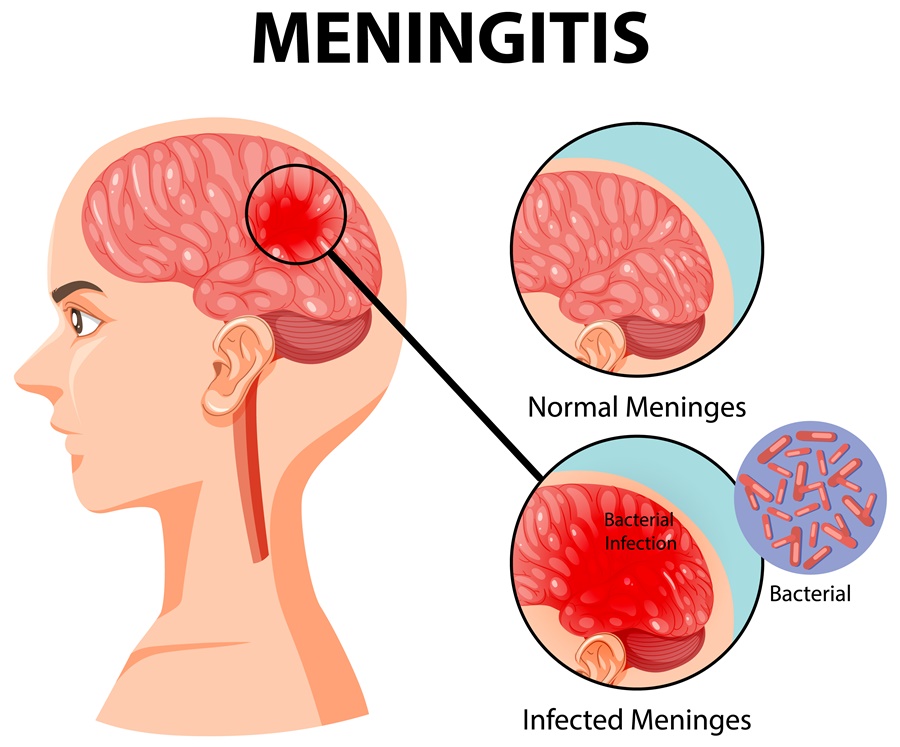
Meningitis is a medical condition characterized by inflammation of the protective membranes covering the brain and spinal cord, known as the meninges. The condition can be caused by infections (bacterial, viral, fungal, or parasitic) or non-infectious factors (such as autoimmune disorders or drug-induced reactions). It is a potentially life-threatening condition requiring prompt medical attention.
Types of Meningitis
1. Bacterial Meningitis
This is the most severe form of meningitis, caused by bacteria such as Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae. It progresses rapidly and can result in serious complications, including brain damage, hearing loss, or death if not treated promptly.
2. Viral Meningitis
Viral meningitis is more common but generally less severe than bacterial meningitis. It is often caused by enteroviruses, herpes simplex virus, or mumps virus. Most people recover without specific treatment, although severe cases may require hospitalization.
3. Fungal Meningitis
This type is less common and usually affects individuals with weakened immune systems, such as those with HIV/AIDS or undergoing chemotherapy. The primary causative agents include Cryptococcus and Histoplasma fungi.
4. Parasitic Meningitis
Parasitic meningitis is rare but can be deadly. It is often linked to exposure to contaminated water sources containing Naegleria fowleri, a brain-eating amoeba.
5. Non-Infectious Meningitis
This form can occur due to autoimmune diseases, certain medications, cancer, or head injuries. Though not caused by an infection, it can present similar symptoms and requires medical evaluation.
Common Symptoms of Meningitis
The symptoms of meningitis can vary depending on the cause and severity. Common symptoms include:
- High fever and chills
- Severe headache
- Stiff neck (a hallmark sign of meningitis)
- Nausea and vomiting
- Sensitivity to light (photophobia)
- Altered mental status, confusion, or difficulty concentrating
- Seizures in severe cases
- Skin rash (common in meningococcal meningitis)
- Sleepiness or difficulty waking up
In infants and young children, symptoms may include irritability, poor feeding, a bulging fontanelle (soft spot on the head), and difficulty waking.
How is Meningitis Diagnosed?
1. Physical Examination
A doctor may check for neck stiffness, altered consciousness, and other neurological symptoms.
2. Lumbar Puncture (Spinal Tap)
A sample of cerebrospinal fluid (CSF) is collected to determine the presence of bacteria, viruses, or fungi.
3. Blood Tests
Blood cultures help identify bacterial or fungal infections in the bloodstream.
4. Imaging Tests
CT scans or MRIs may be performed to assess brain swelling and rule out other conditions.
5. Polymerase Chain Reaction (PCR) Testing
PCR tests detect viral DNA in cerebrospinal fluid to confirm viral meningitis.
Treatment and Management
1. Bacterial Meningitis Treatment
- Intravenous antibiotics (e.g., ceftriaxone, vancomycin) are administered immediately.
- Corticosteroids may be given to reduce inflammation and prevent complications.
- Supportive care such as oxygen therapy and IV fluids may be required.
2. Viral Meningitis Treatment
- Usually self-limiting, requiring rest, hydration, and pain relief.
- Antiviral medications like acyclovir may be used for herpes-related meningitis.
3. Fungal Meningitis Treatment
- Antifungal medications (e.g., amphotericin B, fluconazole) are prescribed.
- Hospitalization is often required for intensive care.
4. Preventive Measures
- Vaccination (meningococcal, pneumococcal, and Hib vaccines) is crucial in preventing bacterial meningitis.
- Good hygiene practices reduce the risk of viral infections.
- Avoiding contaminated water helps prevent parasitic meningitis.
Complications of Meningitis
If untreated, meningitis can lead to severe complications such as:
- Brain damage and cognitive impairment
- Hearing loss or deafness
- Seizures and epilepsy
- Hydrocephalus (fluid buildup in the brain)
- Septicemia (blood poisoning) in bacterial cases
Prognosis and Recovery
The prognosis of meningitis depends on the underlying cause and the timeliness of treatment. While viral meningitis has a high recovery rate, bacterial and fungal meningitis can have lasting complications. Early medical intervention improves outcomes and reduces mortality rates.
Frequently Asked Questions
1. Is meningitis contagious?
Yes, bacterial and viral meningitis can be contagious through respiratory droplets or close contact. Vaccination and hygiene help reduce transmission.
2. Can meningitis be cured?
Bacterial and fungal meningitis require aggressive treatment, while viral meningitis often resolves on its own with supportive care.
3. How long does meningitis recovery take?
Recovery time varies; viral meningitis may resolve within 7–10 days, while bacterial meningitis may take weeks to months, depending on severity.
4. What are the warning signs of meningitis?
A high fever, stiff neck, and severe headache are early signs. Seek medical attention immediately if these symptoms occur.
5. Who is at the highest risk for meningitis?
Infants, elderly individuals, immunocompromised persons, and those in communal living settings are at higher risk.
Meningitis is a serious and potentially fatal condition requiring prompt diagnosis and treatment. Understanding its causes, symptoms, and preventive measures is essential for early intervention and better outcomes. Vaccination and hygiene play crucial roles in preventing certain types of meningitis. If symptoms arise, immediate medical consultation is necessary to reduce complications and improve prognosis.