Medullary Thyroid Carcinoma (MTC) is a rare but aggressive form of thyroid cancer that originates from the parafollicular C cells of the thyroid gland. Unlike other types of thyroid cancer, MTC is characterized by the overproduction of calcitonin, a hormone involved in calcium homeostasis. It accounts for approximately 3-5% of all thyroid cancers and can occur sporadically or as part of a hereditary syndrome.
Causes and Risk Factors
1. Genetic Mutations and Inheritance
MTC is strongly associated with mutations in the RET proto-oncogene. This mutation is responsible for the hereditary form of MTC, known as Multiple Endocrine Neoplasia type 2 (MEN2), which is subdivided into:
- MEN2A: Involves MTC, pheochromocytoma, and hyperparathyroidism.
- MEN2B: Includes MTC, pheochromocytoma, and distinctive physical features such as marfanoid habitus.
2. Sporadic vs. Familial MTC
- Sporadic MTC: Accounts for about 75% of cases and occurs without a family history.
- Familial MTC (FMTC): Inherited as an autosomal dominant condition, typically presenting in multiple family members.
Symptoms of Medullary Thyroid Carcinoma
MTC symptoms can vary depending on the stage of the disease but commonly include:
- A painless thyroid nodule or lump
- Hoarseness or voice changes due to vocal cord involvement
- Difficulty swallowing (dysphagia)
- Persistent neck pain
- Diarrhea (due to excessive calcitonin production)
- Flushing and facial redness
Diagnosis of Medullary Thyroid Carcinoma
1. Blood Tests
- Serum Calcitonin: Elevated levels are a hallmark of MTC.
- Carcinoembryonic Antigen (CEA): Used as a tumor marker to monitor disease progression.
- Genetic Testing: Screening for RET mutations in patients with familial history.
2. Imaging Techniques
- Ultrasound: First-line imaging to evaluate thyroid nodules.
- Fine Needle Aspiration (FNA) Biopsy: Helps confirm malignancy but may not always be conclusive.
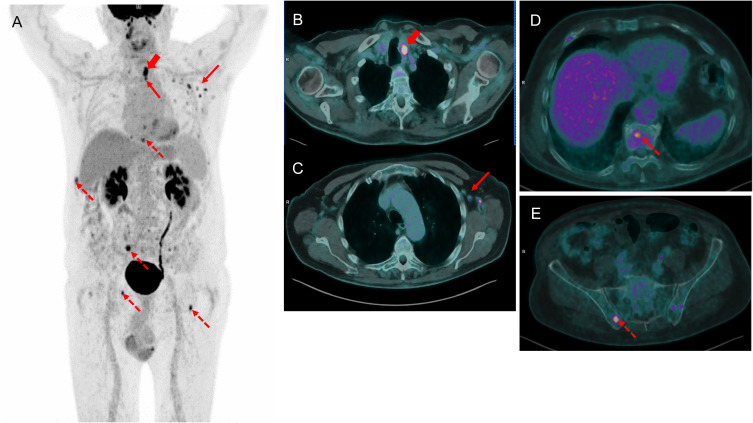
- CT Scan/MRI: Used for staging and detecting metastases.
- PET Scan: Assesses disease spread in advanced cases.
Treatment Options for MTC
1. Surgical Management
- Total Thyroidectomy: Standard treatment to remove the thyroid gland.
- Lymph Node Dissection: Performed if metastases are suspected in cervical lymph nodes.
2. Targeted Therapy
For patients with advanced or metastatic MTC, targeted therapies include:
- Vandetanib: An FDA-approved tyrosine kinase inhibitor (TKI) that blocks RET and VEGFR pathways.
- Cabozantinib: Another TKI effective against progressive MTC.
3. Radiation Therapy
- External beam radiation therapy (EBRT) may be considered for palliative treatment in cases with local recurrence or metastasis.
4. Chemotherapy
- Traditional chemotherapy is generally ineffective but may be used in aggressive cases.
Prognosis and Long-Term Outlook
The prognosis of MTC depends on factors such as tumor stage, presence of distant metastases, and genetic involvement.
Survival Rates
- Localized MTC: 10-year survival rate > 90%
- Regionally Spread MTC: 10-year survival rate ~75%
- Distant Metastases: 10-year survival rate < 40%
Early detection, surgical intervention, and genetic counseling significantly improve outcomes.
Medullary Thyroid Carcinoma is a distinct and complex thyroid cancer that requires specialized diagnostic and treatment approaches. Advances in genetic testing and targeted therapies continue to enhance survival rates and quality of life for affected patients. Regular screening in high-risk individuals is crucial for early intervention and improved prognosis.