Macular edema is a leading cause of vision impairment in patients with non-infectious uveitis. It occurs when fluid accumulates in the macula, leading to swelling and blurred vision. Uveitis, an inflammatory condition affecting the uveal tract, can be of infectious or non-infectious origin. In cases of non-infectious uveitis, immune system dysregulation plays a key role in triggering inflammation and subsequent macular edema.
Understanding Non-Infectious Uveitis
Non-infectious uveitis is an intraocular inflammatory disorder that is not caused by bacterial, viral, fungal, or parasitic infections. Instead, it is often linked to autoimmune diseases such as:
- Ankylosing spondylitis
- Sarcoidosis
- Behçet’s disease
- Juvenile idiopathic arthritis (JIA)
- Vogt-Koyanagi-Harada (VKH) disease
The condition may be classified based on the anatomical location of inflammation:
- Anterior uveitis (most common, affecting the front of the eye)
- Intermediate uveitis (involves the vitreous and ciliary body)
- Posterior uveitis (affects the retina and choroid)
- Panuveitis (involves all parts of the uveal tract)
Pathophysiology of Macular Edema in Non-Infectious Uveitis
Macular edema results from the breakdown of the blood-retinal barrier due to persistent inflammation. This leads to increased vascular permeability, allowing fluid to leak into the macula. Pro-inflammatory cytokines, such as interleukin-6 (IL-6) and vascular endothelial growth factor (VEGF), contribute to this process.
Symptoms of Macular Edema in Non-Infectious Uveitis
Patients with macular edema due to uveitis may experience:
- Blurred or distorted vision
- Reduced central vision
- Increased sensitivity to light
- Difficulty reading or recognizing faces
- Colors appearing washed out
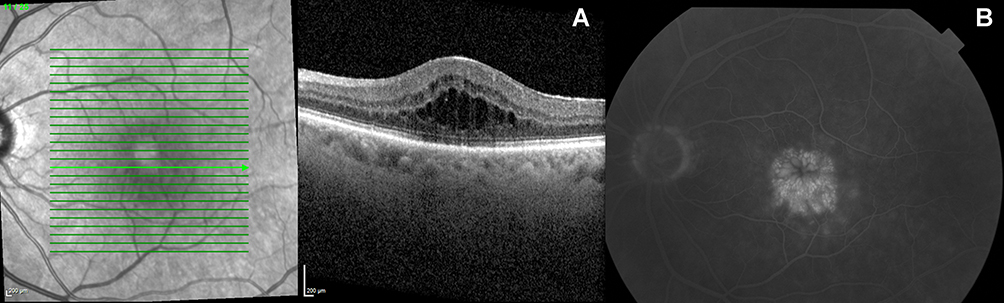
Diagnostic Approaches
Early and accurate diagnosis is crucial for preventing vision loss. Key diagnostic tools include:
- Optical Coherence Tomography (OCT): Provides high-resolution imaging of macular thickness and fluid accumulation.
- Fluorescein Angiography (FA): Detects vascular leakage in the retina.
- Indocyanine Green Angiography (ICGA): Helps identify choroidal involvement.
- Fundus Examination: Evaluates the extent of retinal inflammation.
Treatment Options for Macular Edema Associated with Non-Infectious Uveitis
Treatment strategies aim to control inflammation and reduce macular swelling.
1. Corticosteroid Therapy
- Topical corticosteroids (e.g., prednisolone acetate) for anterior uveitis.
- Periocular or intravitreal corticosteroids (e.g., triamcinolone acetonide, dexamethasone implant) for localized treatment.
- Systemic corticosteroids (e.g., prednisone) for severe cases.
2. Immunomodulatory Therapy (IMT)
- Non-biologic agents: Methotrexate, azathioprine, mycophenolate mofetil.
- Biologic agents: Tumor necrosis factor-alpha (TNF-α) inhibitors like adalimumab or interleukin inhibitors (e.g., tocilizumab) for refractory cases.
3. Anti-VEGF Therapy
- Intravitreal injections of ranibizumab or aflibercept help reduce vascular permeability and fluid accumulation.
4. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
- Oral or topical NSAIDs like ketorolac may provide additional benefits in reducing inflammation.
5. Surgical Interventions
- Vitrectomy: Considered for chronic, non-resolving cases where inflammatory debris affects vision.
Prognosis and Long-Term Management
The prognosis depends on early diagnosis and effective treatment. Long-term monitoring with OCT and regular ophthalmologic assessments is essential to prevent recurrences and complications like retinal scarring or permanent vision loss.
Macular edema in non-infectious uveitis is a serious condition that requires prompt intervention to prevent visual deterioration. With advancements in imaging and targeted therapies, personalized treatment approaches can significantly improve outcomes. Patients should seek regular follow-ups to manage inflammation effectively and maintain optimal visual health.