Androgen deprivation therapy (ADT) is a cornerstone treatment for advanced prostate cancer, effectively reducing testosterone levels to slow cancer progression. However, this therapy is associated with significant adverse effects, particularly loss of bone mineral density (BMD), leading to osteoporosis and increased fracture risk. Understanding the mechanisms, risk factors, and preventive strategies is crucial for optimizing patient outcomes.
Mechanism of BMD Loss in ADT
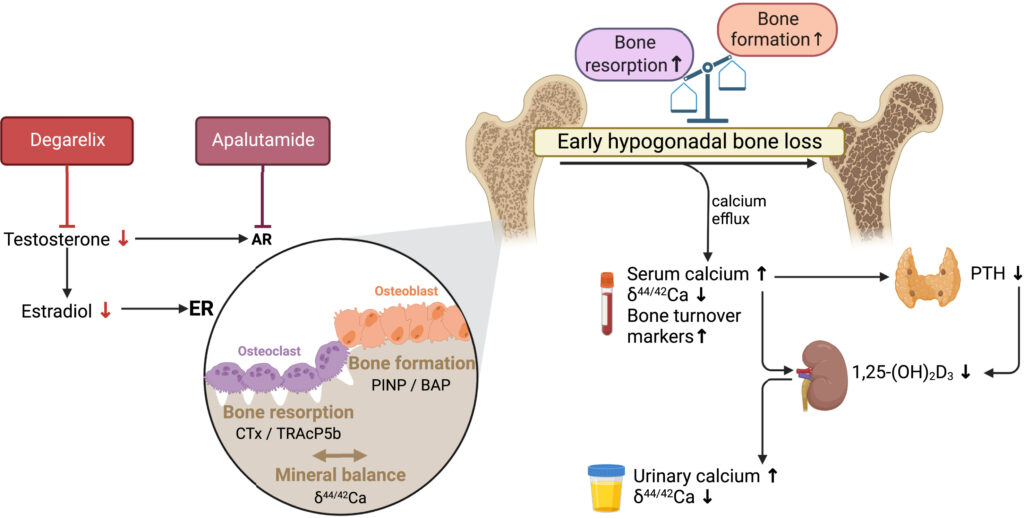
Testosterone plays a critical role in maintaining bone strength by promoting bone formation and inhibiting bone resorption. ADT reduces circulating androgens and estrogens, accelerating bone loss through:
- Increased osteoclastic activity (bone resorption)
- Decreased osteoblastic activity (bone formation)
- Reduced calcium absorption
- Increased urinary calcium excretion
Risk Factors for BMD Loss in ADT Patients
- Duration of ADT: Prolonged therapy leads to greater bone loss.
- Age: Older patients have a higher baseline risk of osteoporosis.
- Baseline BMD: Pre-existing low BMD exacerbates ADT-induced bone loss.
- Lifestyle Factors: Sedentary lifestyle, smoking, and excessive alcohol intake increase risk.
- Comorbidities: Conditions like diabetes and chronic kidney disease negatively impact bone health.
Clinical Consequences of BMD Loss
- Osteoporosis: Severe reduction in BMD, leading to fragile bones.
- Increased Fracture Risk: Higher susceptibility to hip, vertebral, and wrist fractures.
- Reduced Quality of Life: Chronic pain, loss of mobility, and functional decline.
Diagnosis and Monitoring
Regular assessment of bone health in ADT patients is essential. Diagnostic tools include:
- Dual-energy X-ray Absorptiometry (DXA): Standard for measuring BMD.
- FRAX Score: Estimates 10-year fracture risk.
- Bone Turnover Markers: Assess dynamic changes in bone metabolism.
Strategies to Prevent and Treat BMD Loss
1. Lifestyle Modifications
- Weight-bearing exercises: Walking, resistance training, and yoga improve bone strength.
- Smoking cessation and alcohol moderation: Reducing risk factors for osteoporosis.
2. Dietary Interventions
- Calcium intake: Recommended 1000-1200 mg/day through diet or supplements.
- Vitamin D supplementation: Essential for calcium absorption; aim for 800-1000 IU/day.
3. Pharmacologic Interventions
- Bisphosphonates (e.g., Alendronate, Zoledronic Acid): Reduce bone resorption and fracture risk.
- Denosumab: Monoclonal antibody that inhibits osteoclast-mediated bone loss.
- Selective Estrogen Receptor Modulators (SERMs): Beneficial in certain patients.
4. Alternative Androgen-Sparing Therapies
Some emerging treatment strategies aim to balance prostate cancer control with bone preservation, such as intermittent ADT and novel hormone-based therapies.
Loss of bone mineral density due to androgen deprivation therapy is a significant concern for prostate cancer patients, increasing the risk of fractures and associated complications. Early identification, lifestyle modifications, dietary support, and pharmacologic interventions are essential to mitigate these risks. Regular monitoring and a multidisciplinary approach involving oncologists and endocrinologists can help optimize bone health in ADT patients.

