Local anesthesia plays a crucial role in ophthalmologic procedures, providing effective pain relief while maintaining patient consciousness. It offers multiple advantages over general anesthesia, including faster recovery times, reduced systemic risks, and better post-operative patient cooperation. This article explores various local anesthesia techniques used in eye surgeries, their administration, potential complications, and best practices to enhance safety and efficacy.
Types of Local Anesthesia in Ophthalmology
Different types of local anesthesia are employed based on the specific ophthalmologic procedure and patient factors.
1. Topical Anesthesia
Topical anesthesia involves applying anesthetic drops or gels directly onto the ocular surface. It is commonly used for cataract surgery, LASIK, and minor corneal procedures.
Advantages:
- Non-invasive with minimal discomfort
- Rapid onset and fast recovery
- Eliminates risks associated with needle injections
Common Agents:
- Proparacaine (0.5%)
- Tetracaine (0.5%)
- Lidocaine gel (2%)
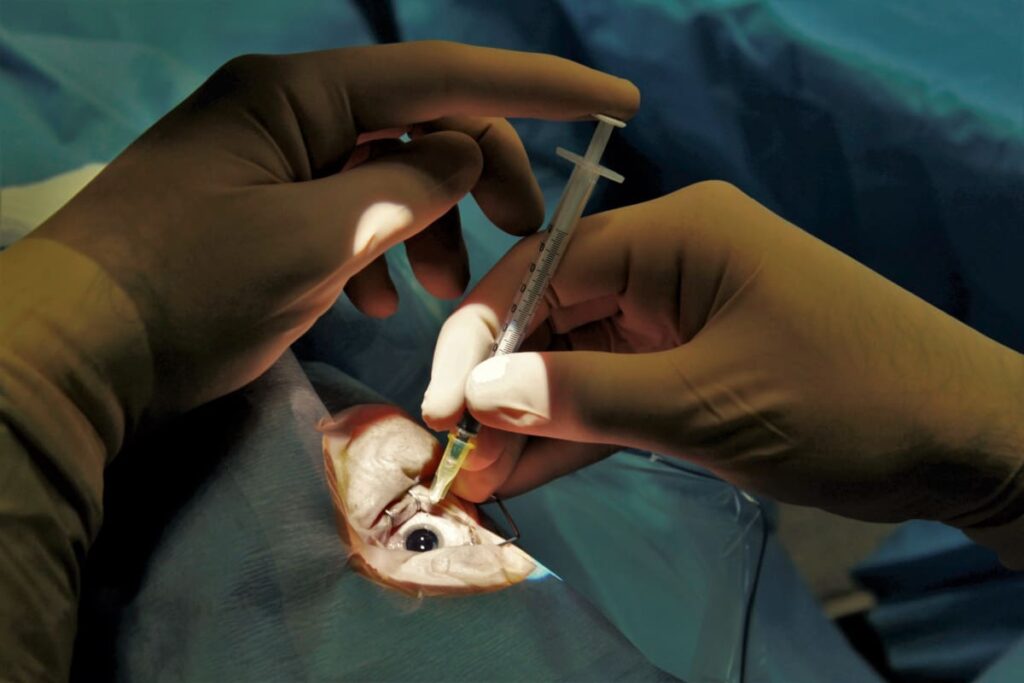
2. Subconjunctival Anesthesia
This technique involves injecting anesthesia beneath the conjunctiva to provide localized pain relief, often used for pterygium surgery and glaucoma procedures.
Advantages:
- Provides deeper and longer-lasting anesthesia than topical agents
- Effective for anterior segment surgeries
3. Retrobulbar Block
A retrobulbar block delivers anesthetic into the retrobulbar space, paralyzing extraocular muscles and ensuring complete analgesia and akinesia.
Procedure:
- A fine needle is inserted through the lower eyelid into the intraconal space
- A mixture of lidocaine (2%) and bupivacaine (0.5%) is injected
- Hyaluronidase is added to enhance diffusion
Advantages:
- Profound anesthesia and complete akinesia
- Suitable for intraocular and posterior segment surgeries
Risks and Complications:
- Retrobulbar hemorrhage
- Optic nerve damage
- Globe perforation
4. Peribulbar Block
A peribulbar block involves injecting anesthesia into the extraconal space, allowing diffusion to the retrobulbar area.
Advantages:
- Safer alternative to retrobulbar block
- Reduced risk of globe perforation
- Good anesthesia and moderate akinesia
Common Agents:
- Lidocaine (2%)
- Bupivacaine (0.5%)
- Ropivacaine (0.75%)
5. Sub-Tenon’s Anesthesia
This technique involves inserting a blunt cannula into the sub-Tenon’s space and administering local anesthetic.
Advantages:
- Minimally invasive with low risk of complications
- Suitable for both anterior and posterior segment procedures
- Reduces systemic side effects
Common Agents:
- Lidocaine (2%)
- Bupivacaine (0.5%)
Best Practices for Local Anesthesia in Eye Surgery
Ensuring safety and efficacy during local anesthesia administration is critical.
1. Preoperative Assessment
- Evaluate patient history (coagulation disorders, allergies, systemic diseases)
- Assess ocular anatomy and previous surgical history
2. Anesthetic Selection
- Consider factors such as procedure duration and patient sensitivity
- Use epinephrine-containing agents cautiously in patients with cardiovascular issues
3. Injection Technique Optimization
- Use fine-gauge needles to minimize trauma
- Avoid excessive pressure to prevent complications like retrobulbar hemorrhage
4. Monitoring and Patient Comfort
- Continuously monitor vital signs
- Provide mild sedation if needed
Complications and Risk Management
Despite its advantages, local anesthesia can lead to complications requiring prompt intervention.
Common Risks:
- Allergic reactions: Rare but possible with ester-based anesthetics
- Globe perforation: Prevent by proper needle positioning and technique
- Oculocardiac reflex: Managed with IV atropine if necessary
Managing Complications:
- Retrobulbar hemorrhage: Immediate orbital compression and observation
- Optic nerve toxicity: Avoid high doses and repeated injections
Local anesthesia in ophthalmologic procedures provides significant benefits in terms of patient safety, comfort, and surgical efficacy. Selecting the appropriate anesthetic technique based on procedural requirements and individual patient factors enhances outcomes while minimizing risks. Proper administration, monitoring, and complication management are essential for ensuring optimal surgical success in ophthalmology.

