Liver transplant rejection occurs when the recipient’s immune system identifies the transplanted liver as foreign and attacks it. Despite immunosuppressive therapy, rejection remains a leading challenge post-transplant. Understanding its causes, symptoms, and treatments is crucial for ensuring transplant success.
Types of Liver Transplant Rejection
1. Hyperacute Rejection
- Occurs within minutes to hours after transplantation.
- Caused by pre-existing antibodies attacking the donor liver.
- Rare due to advanced cross-matching techniques.
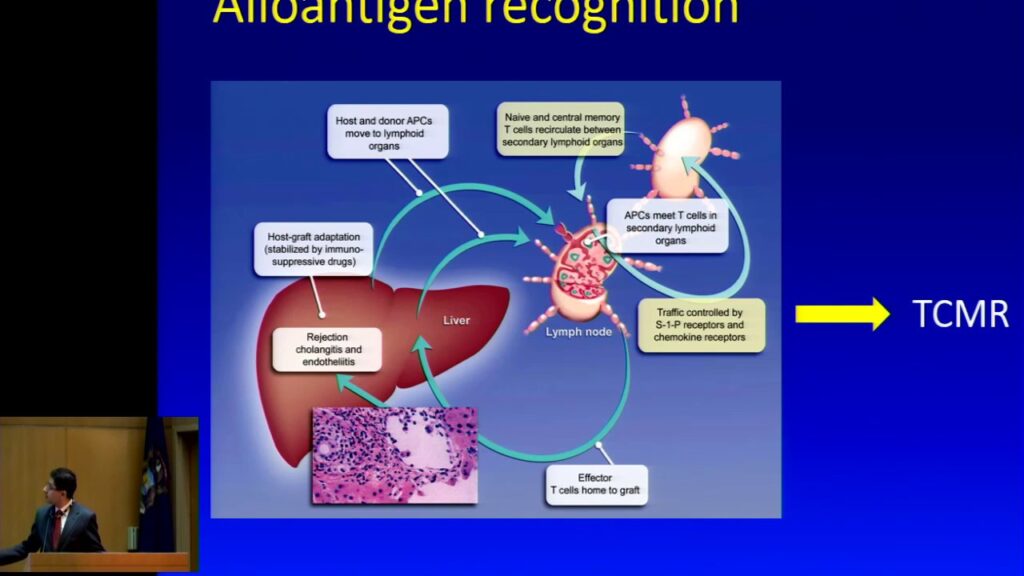
2. Acute Rejection
- Most common within the first three months.
- Caused by T-cell-mediated immune response.
- Often reversible with timely immunosuppressive treatment.
3. Chronic Rejection
- Develops over months or years.
- Leads to progressive loss of liver function due to fibrosis and bile duct damage.
- More challenging to treat, often resulting in graft failure.
Symptoms of Liver Transplant Rejection
- Fever and flu-like symptoms
- Fatigue and weakness
- Abdominal pain or swelling
- Jaundice (yellowing of skin and eyes)
- Dark urine and pale stools
- Nausea, vomiting, and loss of appetite
- Elevated liver enzyme levels
Causes and Risk Factors
- Inadequate immunosuppressive therapy: Non-adherence to medication increases rejection risk.
- Infections: Can trigger an immune response.
- Genetic incompatibility: Some HLA mismatches increase the risk.
- Prior transplant rejection: A history of organ rejection raises susceptibility.
- Donor-specific antibodies (DSAs): Can target the transplanted liver.
- Age and comorbidities: Older age and conditions like diabetes affect immune response.
Diagnosis of Liver Rejection
1. Liver Function Tests (LFTs)
- Elevated ALT, AST, bilirubin, and alkaline phosphatase levels suggest rejection.
2. Imaging Studies
- Ultrasound and MRI assess bile ducts and blood flow.
3. Liver Biopsy
- Gold standard for confirming rejection.
- Helps determine rejection type and severity.
Prevention Strategies
- Strict Immunosuppressant Adherence: Medications like tacrolimus, cyclosporine, and mycophenolate mofetil are crucial.
- Regular Medical Check-ups: Monitoring liver function and antibody levels.
- Lifestyle Modifications: Healthy diet, avoiding alcohol, and infection control.
- Personalized Medication Regimens: Adjusting doses based on immune response.
Treatment Options
1. Medication Adjustment
- Increasing immunosuppressants like corticosteroids.
- Switching to alternative drugs if side effects occur.
2. Plasmapheresis
- Removes donor-specific antibodies from the bloodstream.
3. Biologic Therapies
- Use of monoclonal antibodies (e.g., rituximab) to suppress immune response.
4. Re-Transplantation
- Last resort in cases of irreversible rejection.
Prognosis and Long-Term Outlook
With early detection and appropriate treatment, acute rejection is often reversible. Chronic rejection poses a higher risk of transplant failure, requiring vigilant monitoring. Long-term survival rates have improved due to advances in immunosuppression and transplant care.
Liver transplant rejection remains a serious complication but can often be managed with timely intervention. Adherence to immunosuppressive therapy and regular follow-ups are key to ensuring transplant success. Patients should stay informed about symptoms and maintain a proactive approach to post-transplant care.