Amoebic liver abscess (ALA) is a severe complication of amebiasis, caused by the protozoan parasite Entamoeba histolytica. The infection primarily spreads through the ingestion of contaminated food or water, leading to intestinal colonization and eventual hepatic invasion. If left untreated, it can result in life-threatening complications such as rupture, peritonitis, and sepsis.
Causes and Pathophysiology
1. Transmission and Infection Cycle
Entamoeba histolytica is transmitted through the fecal-oral route via ingestion of cysts present in contaminated food or water. The parasite follows these stages:
- Ingestion of Cysts → Cysts reach the small intestine.
- Excystation → Trophozoites emerge and colonize the colon.
- Intestinal Invasion → Trophozoites penetrate the intestinal mucosa, causing dysentery.
- Hematogenous Spread → Trophozoites enter the portal circulation and reach the liver.
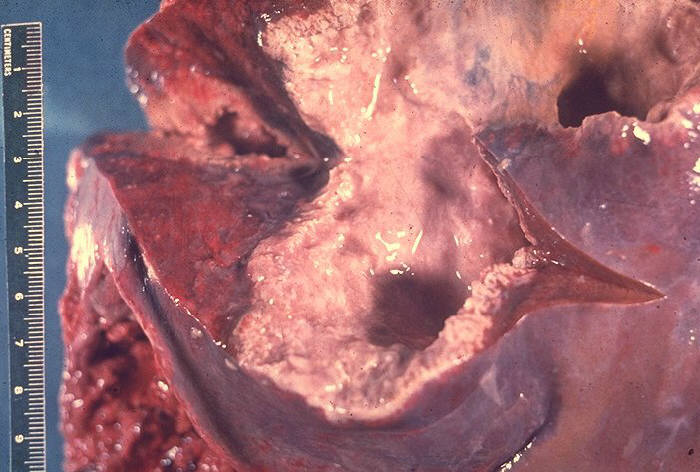
- Liver Abscess Formation → Necrotic liquefaction of hepatic tissue results in an abscess.
2. Risk Factors for Amoebic Liver Abscess
- Poor sanitation and contaminated drinking water
- Travel to or residence in endemic regions (South Asia, Africa, Latin America)
- Malnutrition and immunosuppression
- Chronic alcohol consumption
- Male gender (higher prevalence in men aged 20-50)
Symptoms and Clinical Presentation
1. Common Symptoms
✔ High fever with chills
✔ Right upper quadrant (RUQ) abdominal pain
✔ Nausea and vomiting
✔ Anorexia and weight loss
✔ Malaise and fatigue
2. Severe Symptoms and Complications
✔ Jaundice (suggests biliary involvement)
✔ Pleuropulmonary involvement (cough, pleural effusion)
✔ Rupture of the abscess (peritonitis, septic shock)
Patients with ALA typically do not present with concurrent intestinal symptoms, as hepatic invasion often occurs weeks after initial infection.
Diagnosis of Amoebic Liver Abscess
1. Laboratory Tests
- Complete Blood Count (CBC): Leukocytosis with neutrophilia
- Liver Function Tests (LFTs): Elevated alkaline phosphatase, mild bilirubin increase
- Serology for E. histolytica: ELISA, PCR, or indirect hemagglutination test
- Stool Examination: May detect E. histolytica cysts in the intestines
2. Imaging Studies
- Ultrasound (USG): Hypoechoic, well-defined abscess lesion
- CT Scan: Provides detailed visualization of size and number of abscesses
- MRI: Used for complex or atypical cases
3. Differentiating ALA from Pyogenic Liver Abscess
- ALA: Single lesion (right lobe), serology positive for E. histolytica, no bacterial growth in culture
- PLA: Multiple abscesses, positive blood cultures, high fever with more systemic toxicity
Treatment Options
1. Pharmacological Treatment
- Metronidazole (750 mg TID for 10 days) – First-line therapy for E. histolytica trophozoites.
- Tinidazole (2 g once daily for 5 days) – Alternative to metronidazole.
- Paromomycin (25-30 mg/kg for 7 days) – Eliminates intestinal cysts, preventing recurrence.
2. Drainage Procedures
- Percutaneous Needle Aspiration (PNA): Indicated if abscess is large (>5 cm), refractory to medical treatment, or at risk of rupture.
- Percutaneous Catheter Drainage (PCD): Preferred in multiloculated or complicated cases.
- Surgical Drainage: Rarely needed unless rupture occurs.
3. Supportive Care
✔ IV fluids and electrolyte balance
✔ Pain management with NSAIDs
✔ Nutritional support for recovery
Prevention Strategies
1. Hygiene and Sanitation
✔ Drinking boiled or filtered water
✔ Proper handwashing practices
✔ Avoiding raw vegetables in endemic areas
2. Preventing Recurrence
✔ Complete treatment with Paromomycin to eradicate intestinal cysts
✔ Early treatment of asymptomatic carriers in endemic areas
✔ Improved waste disposal systems in affected communities
Complications of Untreated Amoebic Liver Abscess
✔ Abscess Rupture → Peritonitis, pleural empyema, cardiac tamponade
✔ Sepsis and Multi-Organ Failure → Systemic infection, septic shock
✔ Persistent Liver Damage → Fibrosis, hepatic dysfunction
Amoebic liver abscess is a serious but treatable condition caused by Entamoeba histolytica. Early diagnosis with serological and imaging studies is crucial for timely intervention. First-line treatment includes metronidazole followed by luminal agents like paromomycin to prevent recurrence. Preventive measures, including improved hygiene and sanitation, remain the most effective strategy in reducing disease burden in endemic areas.