Listeria osteomyelitis is a rare but significant infectious disease caused by Listeria monocytogenes, a gram-positive bacterium primarily associated with foodborne illnesses. While Listeria infections commonly lead to meningitis and septicemia, cases of osteomyelitis are infrequent yet severe, necessitating prompt diagnosis and treatment.
Epidemiology and Risk Factors
Listeria infections predominantly affect individuals with weakened immune systems, including:
- Neonates and the elderly
- Pregnant women
- Patients with diabetes, malignancies, or organ transplants
- Individuals receiving immunosuppressive therapy
- Those with prior orthopedic trauma or surgical implants
Though osteomyelitis caused by L. monocytogenes is uncommon, its ability to invade bone tissue makes it a crucial differential diagnosis in immunocompromised patients presenting with bone pain and fever.
Pathogenesis of Listeria Osteomyelitis
Listeria osteomyelitis occurs when L. monocytogenes reaches the bone, primarily through:
- Hematogenous Spread: Bacteria enter the bloodstream, seeding into the bone marrow.
- Direct Inoculation: Trauma, surgery, or open fractures introduce the pathogen.
- Contiguous Spread: Infection spreads from adjacent soft tissues or joints.
Clinical Manifestations
The presentation of Listeria osteomyelitis varies but typically includes:
- Persistent bone pain and localized tenderness
- Fever, chills, and malaise
- Swelling and erythema over affected bone
- Reduced range of motion if joints are involved
In neonates and immunocompromised individuals, symptoms may be non-specific, increasing diagnostic challenges.
Diagnosis
Early detection of Listeria osteomyelitis is critical for effective treatment. Key diagnostic methods include:
Laboratory Tests
- Blood Cultures: Identifies L. monocytogenes in systemic circulation
- Inflammatory Markers: Elevated CRP and ESR suggest infection
- Joint Aspirate Analysis: In cases with concurrent septic arthritis
Imaging Studies
- X-rays: May reveal periosteal reaction or bone destruction in advanced cases
- MRI: Gold-standard imaging for detecting early osteomyelitis
- CT Scan: Useful for assessing bone involvement and abscess formation
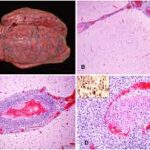
- Bone Biopsy and Culture: Definitive diagnosis via histopathological analysis
Treatment Strategies
Listeria osteomyelitis requires prolonged antimicrobial therapy combined with surgical intervention in severe cases.
Antibiotic Therapy
- First-Line Treatment: High-dose IV ampicillin or penicillin G
- Alternative Therapy: Trimethoprim-sulfamethoxazole (TMP-SMX) for penicillin-allergic patients
- Duration: Typically 6–8 weeks, with initial IV therapy followed by oral antibiotics
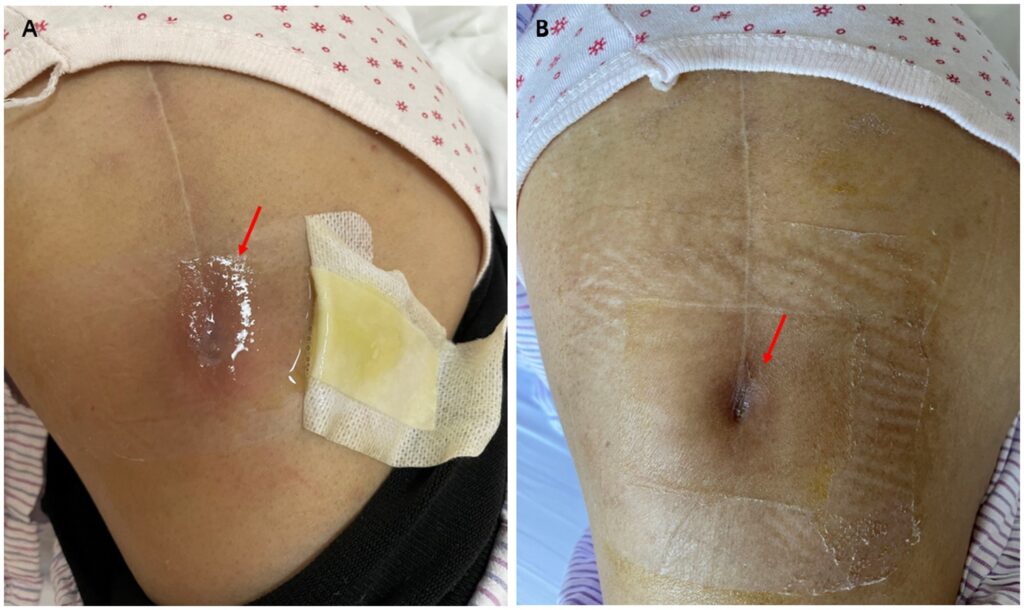
Surgical Management
- Debridement: Removal of necrotic bone tissue
- Drainage: For abscess formation
- Implant Removal: If orthopedic hardware is infected
Prognosis and Complications
Early treatment leads to favorable outcomes; however, delayed diagnosis can result in:
- Chronic osteomyelitis
- Pathological fractures
- Septic arthritis
- Systemic complications such as sepsis
Prevention and Public Health Considerations
Preventing Listeria infections, including osteomyelitis, involves:
- Proper food hygiene to avoid listeriosis (avoiding unpasteurized dairy and undercooked meats)
- Monitoring immunocompromised patients for early signs of infection
- Prompt treatment of systemic Listeria infections to prevent hematogenous spread
Listeria osteomyelitis is a rare but severe manifestation of L. monocytogenes infection. Due to its nonspecific symptoms and potential for complications, high clinical suspicion, rapid diagnostic evaluation, and aggressive treatment are essential. Continued research into antibiotic efficacy and infection control measures remains crucial for improving patient outcomes.